NHS England’s National Director of Operations and Information has publicly named and shamed a number of trusts that he claimed were failing to submit referral to treatment (RTT) reports.
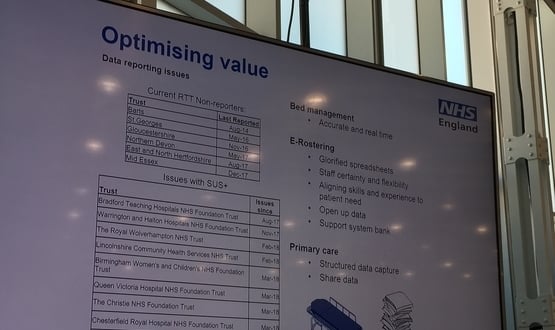
Speaking on the first day of UK e-health Week 2018 on 15 May, Matthew Swindells said that despite the NHS investing “millions of pounds in technology”, there was still six trusts that were not disclosing their waiting lists to NHS England frequently enough.
This included Barts Health NHS Trust, which Swindells said had not sent an RTT report since August 2014.
Board papers from May show the trust has suffered from issues “relating to the accuracy of waiting list data”.
In a statement the trust said: “Barts Health NHS Trust has rectified long-standing issues with its systems used to report waiting list information, meaning we intend to publish waiting times for routine and non-urgent conditions from June to reflect waiting times from April 2018 onwards.”
The other trusts that were called out included:
- St George’s University Hospitals NHS Foundation Trust
- Gloucestershire Hospitals NHS Foundation Trust
- Northern Devon Healthcare NHS Trust
- East and North Herts NHS Trust
- Mid Essex Hospital Services NHS Trust
RTT reports include data which indicate how trusts are delivering on a patient’s right to receive treatment within 18 weeks of being referred to a consultant-led service.
Swindells said it was “not acceptable” that the named trusts were failing to submit such reports, going so far as to tell members of the audience belonging to these trusts to go back to the office and “get to work” after his presentation.
He said: “We walk around most hospitals and we’ve not known how many beds we have and how many patients are lying in them.”
“We need to at the very least get the data that we capture back out. If we can’t do the basics, me going cap-in-hand to the treasury for another £10bn to sort IT out just sounds like fool’s money.”
“We have to get this bloody stuff right”, he said, adding that NHS England’s failure to “deliver competent and basic IT” was preventing it from “running a sufficient NHS”.
A spokesperson for St George’s said the trust’s suspension of RTT reporting was ‘2016 due to significant data quality concerns’.
They added: “Our Elective Care Recovery Programme was set up shortly after to tackle our data quality challenges, and to ensure patients aren’t waiting longer than they should for treatment.
“We made clear at the outset that there will be no quick fix to the data quality challenges we face, but we have made significant progress – including the introduction of a new waiting list management system at St George’s Hospital (Tooting).
“Work continues to address our data quality challenges, and to return to national reporting in the future.”
When contacted for comment, a spokesperson for Northern Devon Healthcare NHS Trust said: “In June 2017 we agreed with NHS Improvement to temporarily suspend the national reporting of RTT whilst we improved the quality of RTT data and validation, following the implementation of our new electronic health record.
“Since then, we have been working through our plan to resolve the data validation issues and have made significant progress. We are looking to restart reporting RTT data very soon.”
According to Swindells, NHS England’s ten-year vision for the future includes becoming a “data-led” organisation that supports new innovation and puts the “consumer at the forefront”.
Swindells previously caused a stir when he said the NHS’s digital best were ‘mediocre’ by international standards.

25 May 2018 @ 07:39
I suppose Tesco would have similar problems if their POS systems were all different. Some good, some poor and variations in how the staff use them.
The IT will only show what is in the system. Get the data right as it goes in and there’s less need to sort and tidy it up as the quality of collection improves. Error trapping and validation rules help but beware of those using the system who will always try to find an easier way of doing their tasks. If the system has loopholes in the logic, staff will find and use them.
Lastly, validation of the queries used to pull the data out of the system is essential. What constitutes the population of the data, what are the rules for diminishing the population and what order do the need to be applied. It sounds simple but get it wrong and your data is invalid.
22 May 2018 @ 11:28
I do not believe it is the healthcare systems that are really at fault here. The issues lie with poor data being migrated and then the issue being compounded when these new systems enforce the correct governance.
Trusts are continually advised and encouraged to clean up poor data before it is migrated but often fail to do this, where trusts have taken on board this advice the issues they have experienced are significantly less.
The short sighted approach of some trusts not to invest in this critical exercise is now coming back to haunt them.
18 May 2018 @ 15:31
Great observations from Matthew Swindells on the challenges faced by the NHS in submitting statutory returns.
Working with the NHS we see the struggles many face to not only deliver a great patient experience, and meet the constitutional right for patients to be seen within the 18 week period, but also to deliver national reporting.
The widespread use of inefficient and often dated systems to manually manage patient tracking and RTT frequently adds to the time and costs incurred in managing elective care and submitting these reports as well as issues with data quality.
We know from working with leading GDEs that investing in the use of sustainable technologies to automate the creation of a single view of patient pathways delivers cost, time and operational efficiencies.
Managing patient pathway data in this way ensures that not only are you managing pathways to improve patient experience but to also resolve the root cause of data quality issues. In addition using such technologies enables trusts to easily and quickly create accurate, timely and evidenced statutory reports.
http://www.insource.co.uk
17 May 2018 @ 22:01
The IT systems at these Trusts:
Cerner
Cerner
Intersystems
Intersystems
CSC Lorenzo
CSC Lorenzo
It seems unfortunate that these expensive systems from large US corporations cannot deliver basic operational data. Let’s hope Private Eye doesn’t get hold of this!
25 May 2018 @ 07:42
I would ask which other organisations are using the same systems and submitter urns successfully? You cannot blame the system if some trusts have got it working.
17 May 2018 @ 15:55
How many of the Trusts failing to submit RTT data have had this issued caused by the implementation of a new PAS system?
21 May 2018 @ 11:52
This issue has been covered by Private Eye’s Medicine Balls several times in the past.
Other Trusts using these systems have been routinely submitting SUS and RTT data returns for several years – why these haven’t seems to be down to data quality issues.
The old adage “garbage in, garbage out” springs to mind.
22 May 2018 @ 15:23
Without wanting to split hairs, Lorenzo was first developed for the NHS and Trakcare isn’t sold in the US, so the link to US companies is erroneous.
I couldn’t agree more with ABC’s comments and it bears out time after time.
What I would also say is that data migration is part of the problem, but the other aspect is that reporting and testing are often not adequately addressed adequately as part of data migration strategies. That is then compounded when the broader data migration workstream is not fully integrated into the EPR/PAS implementation team.
22 May 2018 @ 16:43
Completed agree JAJ, ABC and Ex NHS Techie –
I understand that the TrakCare data migration programme/process is well structured and that InterSystems provides tools to enable Trust’s to migrate data repeatedly (like once/twice per week right up to go-live) over the course of the implementation into test environments, where it is then made available to the EPR/PAS programme teams, Trust “super users” and local Information Teams. Given that most of these implementations take around 12-18 months to complete (rather optimistic, I know), that is roughly a minimum of 104 (crudely based on 52 weeks * 2 migrations per week) data migrations during the EPR implementation which should be adequate to address any DQ issues, just as long as the organisation recognises that it is has a collective responsibility to “get eyes on the data”.
It goes without saying that it takes an enormous amount of effort/resource to do this and that, arguably, to do it successfully requires the total support of an organisation, right up to board level (and by support I mean acceptance of the fact that other “pet” projects go on hold whilst this work is given the highest of priorities). I guess the data migration/EPR teams at the Trusts who use the same software but haven’t experienced these issues, had this support (whilst also being technically savvy, knew their organisation’s data well and ensured their migrated data was tested at every step of the process throughout the implementation etc.)
And no, I have not and do not work for InterSystems – I just share the same view as ABC that the healthcare systems are not at fault here.
17 May 2018 @ 10:43
Seems rather unfair to berate trusts regarding the billions spent to little effect – that was very much central government policy, and I am sure the trusts would have preferred to get their hands on the money to put it to good use.
It baffles me as to why NHS England is still requiring a separate submission of RTT data, when all of this data is supposed to be in SUS.
22 May 2018 @ 10:06
RTT is perhaps the least of Gloucester’s worries, if this is to be believed: http://www.bbc.co.uk/news/uk-england-gloucestershire-44052432
As far as one can see, or indeed have heard, the other trusts using the same TrakCare software have not reported either the problem identified in the BBC article or issues with submitting Referral to Treatment returns.
17 May 2018 @ 10:37
I want to share my story what nhs hospital did with me abusing inside the hospital damage my more body refuse to give me pain relief in my body this Hospital Staff do not have any manners the mislead to the patient about blood test they send me home 36 time with infection lie to me I am suffering so much home I am very scared with this Hospital I stop going to the hospital for further treatment this hospital belong to Essex many thanks