Three things we must do now to prevent patient harm from digital tech
- 25 June 2024

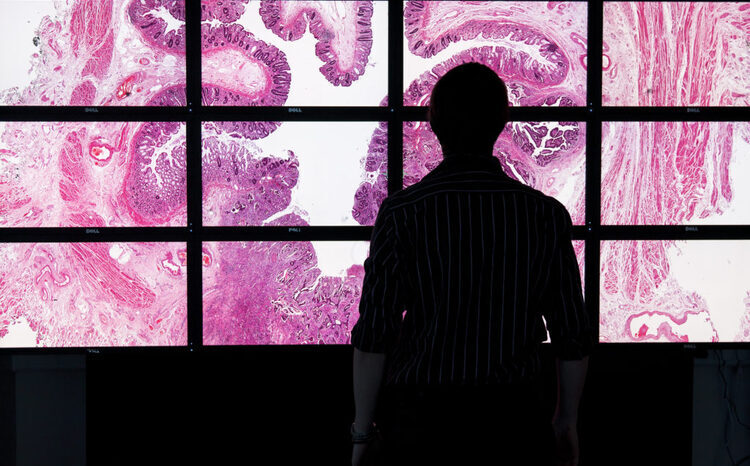
In the wake of reports linking IT flaws to deaths of patients and the recent cyber attack on pathology services in south east London, Chris Fleming calls for radical change to make digital safer and more effective
Digital technologies and ways of working have huge potential to transform our healthcare system and alleviate some of the pressures facing the NHS. But only if we do it right.
So how are we getting on? Last month, the BBC reported on IT system failures that have been linked to the deaths of three patients. And in the last fortnight a pathology system supporting some of our biggest hospitals has been taken offline, and an entire healthcare system’s digital infrastructure was reported to have collapsed.
We need to change. We need to improve the products we ask our staff and patients to use, insist that the market modernises alongside us, and recognise that digital is not the same as IT – it changes the way healthcare is delivered. It is essential to get this right, to tackle the risks of digital systems and prevent patient harm.
Reshape the market
It’s tempting to bury the reasons for this failure behind issues of complexity. And in fairness to my colleagues working in the sector, the federated nature of the NHS, and the inherent complexity of medical data and medical practice, are undoubtedly contributing factors.
But the complexity is not a sufficient excuse.
There are three things we can and must do now to mitigate future patient harm and make sure we are leading digital change in the most effective way we can.
Firstly, we must take market shaping seriously to drive drastic improvements in the products we use every day in the NHS. We need to act on rent-seeking behaviours and give new players who are shaping the market in a positive way a boost. Given the general failure of the market to respond to this design challenge (with a few exceptions) we might, as Digital Health’s editor-in-chief Jon Hoeksma points out, be rather better off building some of our own systems.
Secondly, we need to take the development, coordination, and enforcement of open standards in interoperability and cross-institutional communications seriously and underpin it with the resources that reflect its importance. It is an unglamorous topic, but this plumbing is vital for the future of the NHS. The Data Protection and Digital Information Bill, which had provisions for interoperability between vendors, fell down in the wash-up period after the general election was called. If they win the election, as looks likely, Labour should revive the provisions in the Bill, to give the NHS teeth to force interoperability without being scared of the response of the market.
Thirdly, we need to recognise across the NHS that digital health is not about funding ‘IT projects’ but a fundamental rewiring of the way healthcare is delivered, requiring requisite buy-in from the whole organisation both at national and provider level.
Digital at the top table
All of which will require a well-informed and muscular centre playing a servant leadership role with the system. Digital and technology experience should be at the very top table of NHS England. Clear architecture and commercial strategies should be developed in conjunction with the wider NHS CIO community.
NHS England needs to focus on a long-term approach to funding and should build (or fund the scaling of) world leading open platforms that are designed for adoption that can take pain away from the system and prevent the front line from having to constantly reinvent the wheel.
The Wade-Gery review recommended “Putting data, digital and tech at the heart of transforming the NHS”. I know many fantastic people in the local and central NHS who get it and are succeeding, in spite of the challenges. We need to break down the barriers, unblock things for them, and let them deliver.
The complexity of the digitisation of the NHS and social care is such that it is not an area where major systemic change can happen over the short term. This has been proven many times in the past. Any incoming administration would be advised not to underestimate how hard it will be to deliver their technology commitments – especially those involving patient data, as the operational changes are huge.
But if we do not at least start with a radical rethink of how to go about these challenges, history will be doomed to repeat itself.





1 Comments
Amen to this sensible 3 point plan but especially to “shape the market” rather than being shaped by it for another 20 years. Sadly I’m not sure anyone who matters gets it and everyone who does get it, doesn’t matter. Helluva a catch.
Comments are closed.