2008: the year telecare grows up?
- 18 December 2007
 |
From April next year three areas in England will seek to develop a national business case for the use of assistive technology – such as telecare, telehealth and e-health – to support integrated health and social care.
Kent, Newham and Cornwall cover more than a million people between them and will install telecare and telehealth devices in around 7,000 homes, to assess the impact of assistive technology both on people’s lives and on the cost of providing care and support.
The evaluation team for the Whole System Long Term Conditions Demonstrator programme will examine the effects of the technology on emergency admission rates, patient/carer experience, and quality of life, as well as looking at the impact on primary care.
The numbers involved will be far larger than any trial of its kind so far in the UK. The closest England has come to a large scale trial of telehealth has been the work carried out by Kent County Council in conjunction with local PCTs. Over the last two years it has recruited 250 patients who have been using telehealth devices to monitor vital signs such as blood pressure, pulse oximetry and blood glucose levels.
The project operated the telehealth scheme using a range of models and full results are due out at the end of the year. The Kent team says that early results show that of those running the practice-based scheme, two practices using practice nurses, reduced their acute care costs from £43,000 to £10,500 for 15 patients with long term conditions measured, over six months and using conservative costings.
For 60 patients managed by community matrons there was a 60% reduction in acute care costs and 40% reduction in GP contacts.
Lack of evidence restraining investment
Scarcity of UK based evidence about the cost-effectiveness of telecare and telehealth is one factor enthusiasts believe has so far held back investment in assistive technology. This is why the Whole System Demonstrator (WSD) programme is seen as so important.
Charles Lowe, programme director of the Newham Advanced Telecare (NeAT) project and now head of the borough’s WSD site, says: “I’m really hoping that this proves beyond all reasonable doubt that as part of an overall package of improved processes we can have success in improving the level of care that we deliver to people.”
The NeAT project has the largest number of telecare users in England with approximately 2300 installations.
One of the problems with developing evidence for the use of assistive technology has been to separate out the impact of the technology on, for example, emergency admission rates, from a whole range of other initiatives also being targeted at patients with long term conditions such as the community matron programme, the Quality and Outcomes Framework and so on.
Strong potential for the future
Outcomes, however, do look promising. Newham uses a range of telecare devices to support people in their own homes and assesses each person individually. Lowe says that in 2004/5 241 people went into residential homes and in 2005/6 that figure was 124. “I’m absolutely certain telecare contributed to it,” he adds.
Government policy and demographics would also seem to paint a potentially bright future for telecare and telehealth with key policy initiatives across health, housing and social care which aim to bring care into the home, reduce emergency admissions and improvement management of long term conditions.
There are more than 15 million people with LTCs in England and patients with LTCs account for about 80% of GP consultations, are twice as likely to be admitted as an inpatient and stay in hospital for longer. A small proportion of patients also account for a high proportion of use, with 10% of patients accounting for 55% of bed use and 5% of patients accounting for 42% of bed use.
When the white paper Our Health Our Care Our Say was published at the beginning of 2006, the DH promised that the demonstrators would explore the possibilities opened up by integrated health and social care working supported by advanced assistive technologies such as telehealth and telecare.
A DH spokesperson told EHI Primary Care: “The demonstrators will lead to a better understanding of the level of benefit associated with such developments. They will also help fast track future change by addressing key implementation barriers and providing solutions for the wider NHS and social care.”
The successful sites were appointed in May 2007. The DH spokesperson added: “Much work has been undertaken working through the evaluation design with the evaluation consortia, implementing rigorous project management disciplines, as well as developing pathways for the use of the technology and engaging the huge number of stakeholders who will be affected by the demonstrators.”
GPs key to success
Within this group GPs’ engagement is seen as key to the success of the implementation of the programme. Richard Parton, communication and change manager on the telehealth project in Kent, says the project “initially struggled a little bit” with GP engagement but now has GP involvement at a number of levels including a GP on the telehealth project board.
Parton says telehealth offers obvious attractions to practice based commissioning groups seeking to cut emergency admission rates and Dartford, Gravesend and Swanley PBC cluster have been fully involved in the Kent telehealth programme as part of their PBC agreement.
With the biggest experience of telehealth to date, Parton says the project team have built up expertise in what works and what does not when running a telehealth programme.
He adds: “We feel quite strongly that the easiest way to start using telehealth isn’t necessarily the best. Rather than a separate model telehealth should be seen as an additional service which is part of the normal service delivery and is another tool in the range of tools available to a clinician.”
Andrew Forrest, programme director for the Cornwall LTC demonstrator, also emphasises that the ambition of the demonstrator sites is not to use the technology to isolate people but to provide them with support for self management backed up by visits and other, more traditional health and social care interventions.
All three sites will work in the same way although they are procuring their own telecare and telehealth devices from the NHS PASA framework.
In addition to the main programme the demonstrator sites are running additional pilots tailored to their own needs. In Cornwall this will involve recruiting 7500 for ‘light touch’ telehealth delivered via telephone support to patients and in Newham, the project hopes to tackle high rates of diabetes by offering telehealth via mobile phones to around 1000 patients.
The main focus for all three sites, however, is to provide the evidence for more widespread use of telecare and telehealth, a cause they all believe in.
Lowe adds: “I’m absolutely passionately committed to the beneficial use of technology to improve the level of service that we give to the people we help and that is what motivates me in all of this.”
DH definitions on assistive technology
| e-health | Health services, information and education delivered or enhanced through the internet and related technologies. eHealth encompasses telecare, telehealth and telemedicine |
| Telecare | The continuous, automatic and remote monitoring of real-time emergencies and lifestyle changes over time in order to manage the risks associated with independent living |
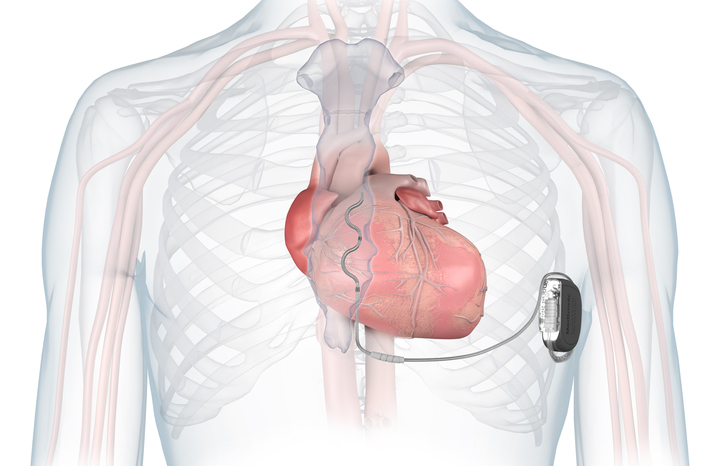
| Telehealth | The delivery of healthcare at a distance using electronic means of communication – usually from service user to clinician eg a service user measuring their vital signs at home and this data being transmitted via a telehealth monitor to a clinician |
| Telemedicine | The delivery of healthcare at a distance using electronic means of communication – usually from one clinician to another eg a non-specialist GP undertaking an ECG on a patient suspected of heart disease and the transfer of that data electronically to another specialist clinician for discussion/comment. |