We’re getting there…
- 2 July 2009
 It’s nine months since University Hospitals of Morecambe Bay NHS Trust became the first acute trust to start deploying Lorenzo, giving it a ‘soft landing’ on one ward at Furness General Hospital. Sarah Bruce recently got on the train to see how much progress it has made in rolling out iSoft’s electronic patient record since then.
It’s nine months since University Hospitals of Morecambe Bay NHS Trust became the first acute trust to start deploying Lorenzo, giving it a ‘soft landing’ on one ward at Furness General Hospital. Sarah Bruce recently got on the train to see how much progress it has made in rolling out iSoft’s electronic patient record since then.
It’s a long way from London to Lancaster, where University Hospitals of Morecambe Bay NHS Trust runs the Lancaster Royal Infirmary. It’s a very long way to Barrow in Furness, where it runs Furness General Hospital.
When one of E-Health Insider’s reporters made the longer trip in October to see Lorenzo given its ‘soft landing’ on one ward of Furness General, she expected to make the shorter trip in the spring to see the start of its roll-out at the Royal Infirmary.
So when another reporter found herself changing trains at Lancaster and getting on a “sprinter” to take her the extra hour up the coast, it was a clear sign that the project had suffered further delays.
Some progress has been made. Lorenzo is now live on all of Barrow’s surgical wards, except for paediatrics and day surgery, and has completed its pilot phase at the hospital. It has also started generating electronic discharge summaries for GPs.
However, a roll-out planned for medical wards in Lancaster is still “two or three months” away. And some of the enthusiasm that was obvious in October seems to have given way to a realisation of just how much hard work still lies ahead.
Dr Sydney Schneidman, consultant in emergency medicine and the trust’s clinical lead for health informatics, admits: “The honeymoon period is over for everyone now and people have started to see Lorenzo as, not a chore, but a challenge.
“People just don’t seem to be grasping that this is extremely advanced computing and not just a project, but a project that is continuously under development.”
Intensive training
Another big challenge has been training. Lynne Atkinson, a nurse and midwife who has been working on the clinical content of Release 1, says Furness General has a long history of using computers, so its staff are used to seeing informatics staff on the wards.
This made it natural for the trust to take an approach to training on Lorenzo that it calls “taking the training to the user.” Atkinson says: “All training is done in round-time, bit by bit, which takes around four hours in total. Everyone has training tailored to their particular job, on the ward, or in a near-by room.”
Steve Fairclough, the trust’s head of informatics, says: “This method of training is very resource intensive from our side, but it doesn’t interrupt the clinicians. Whether it is going to be suitable when we get quicker and begin completing a ward a week, I’m not sure.”
Dr Schneidman adds: “We have a lot of organisational issues, particularly when training juniors, as we have to start at square one every time there is a rotational change.
“So far, we’ve stalled every three months, which is a mixed blessing. It’s inconvenient now, but as the system is rolled out more people will have been trained and then moved on – so eventually it will be a decreasing curve.”
Technical problems with the data center, N3 and the trust’s infrastructure have also contributed to the slow pace of progress.
Still committed to the vision
Nevertheless, the trust and its informatics team is pushing forward with the vision of a single electronic patient record for the whole health community. Those involved in the project remain 100% committed to the National Programme for IT in the NHS, and what Fairclough calls a “transformational service, not an IT project.”
At the moment, the trust is deploying a “general EPR”, which is built around giving clinicians access to information about the patients in their care. Fairclough says this is a “huge facet of the system” and one that makes it easier for clinicians to use.
The system records patient problems on admission, alerts that are relevant to the patient’s state, including behavioral issues and allergies, and provides radiology requesting and associated results.
It also provides electronic discharge summaries which can be sent to GPs within 24 hours and has a built in workflow that enables the discharge process to start days before the patient leaves the hospital.
Alongside the roll-out, the trust is completing fortnightly upgrades, which means reverting back to paper systems for around 12 hours every other weekend.
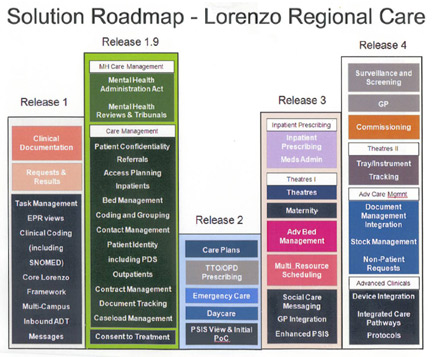
It is also working on a Lorenzo Release 1.9 and Release 2 project, which aims to bring the care management features of R1.9 and the emergency care features of R2 together (a pathway for Lorenzo releases, provided by the trust, can be seen at the end of this feature).
Fairclough hopes to be at Lorenzo Release 3 in 12-18 months. R3 is scheduled to include inpatient prescribing and integrated care pathways, and Fairclough says it should give the functionality the trust joined the national programme for.
Getting over the hump
Ward manager Helen Thompson says Lorenzo is already proving useful to her and her team, as it provides a view of where test orders and results have got to.
However, she says that while they are still excited to be involved in the project, she and her staff are frustrated with the slow implementation and slightly disappointed with the complicated interface.
She says: “This has the potential to be really good. But the truth is that things don’t look like they do in the picture and aren’t as we imagined them to be. We all thought it would look similar to the paper copies, but it’s a lot more clicky and multi-screened, which makes the transition much harder.”
She continues: “There has been some resistance but I think once it becomes inherent practice people will adjust. If nurses can see benefits to patients, they will embrace it.”
And for all the problems and frustrations, Dr Schneidman still believes that if other trusts are reluctant to get involved now, they will pay a higher price in the future.
“The longer people stand off, the harder the harder it’s going to be, and the more behind people will become,” he says. “Those who are implementing their own EPR are only getting a very short term gain.”
As an American, he is particularly concerned that if more trusts don’t jump on board the UK will import some of the problems that the US now has.
“America has very mature IT systems that don’t talk to each other. If that happens here, then it’s going to be very sad. We have a tremendous opportunity here, but people get impatient for whatever reason – and for that, they’re going to lose part of this vision of having a single record for all.”
Stepping up the plate
Fairclough agrees, adding that the NHS needs to “step-up to the plate” in terms of deployment. He says: “We are the only ‘show and tell’ site in the North of England, and hardly anyone has come to visit. People say they have EPR, but its nonsense. What they have is an organisational record.”
Both Dr Schneidman and Fairclough are also concerned about other trusts’ capacity to cope with the scope of Lorenzo. Morecambe Bay has received hundreds of hours of help from NHS Connecting for Health and its local service provider, CSC.
But Fairclough still has around 80 people in his IT department and plans to add around 30 more on short term contracts when the roll out finally begins in Lancaster.
Dr Schneidman adds: “Other trusts have ten people, it would be impossible to implement something of this scale using such a small team. The NHS doesn’t seem to understand what proper service change takes. It’s not just organisational change that’s involved its reengineering of clinical change and a cultural change too. It’s obvious that this was never going to be easy.”
 |
|
Click the image above to view full size. |




