CCIOs in mental health
- 7 August 2012

Thirty plus psychiatrists create a lively hum of conversation in the Marlborough Theatre of the King’s Fund.
Some of those attending the latest CCIO Leaders Network event put their point across more forcefully than others, as they hone in on the gritty detail of the skills that a chief clinical information officer needs.
But no one is short of an opinion. And one thing they all agree on is that the current state of NHS IT deployments is not very good.
21st century IT
Professor Sue Bailey, president of the Royal College of Psychiatrists, gets proceedings going by saying that the CCIO role is invaluable and “will make a great change.”
While some clinicians – and their trusts – see IT as something to be endured, Dr Bailey argues that innovative organisations realise that IT is about “clinical utility of data for improving patient care.” So CCIOs have the scope to determine how their trusts move into the 21st century.
“There will be challenges around information governance, but I think it’s possible to have good governance frameworks for anything,” she tells the audience. “It’s about knowing you have good data and actually using it to benefit patients.”
After her opening address, Dr Bailey tells eHealth Insider that she has noticed a “sea change” in attitudes to IT over the past two to three years.
“They [clinicians] realise IT is here and here to stay,” she says. “Now it’s about how they take some ownership and leadership in this, working with other people with the skill sets needed to deliver it.
“It’s about getting clinicians to feed in what’s needed that will help to improve services for users and carers.”
Clinical input – vital but rare
Involving clinicians from the start of big IT projects seems simple, but projects fall down time and again because they lack clinical engagement, points out EHI editor Jon Hoeksma.
The first tranche of ‘official’ CCIOs will, in most cases, come from the ranks of people who have already been doing the job on an “ad hoc basis.”
But getting trusts to appoint CCIOs, to lead on IT and information projects, will give them status, and encourage other trusts to look for structured clinical support and leadership. “It’s about giving formal recognition,” he says.
Hoeksma adds that CCIOs usually do the role for between two and four days a week but in the US, where the role is more developed, it often becomes full time.
Dr Joe McDonald, a psychiatrist in Newcastle who was national clinical director, mental health, and who is still chair of the British Computer Society mental health specialist group, adds that what a CCIO has to understand is what the different groups in an NHS organisation want.
Put succinctly: “Clinicians just want to write stuff down, managers want to count stuff, and techies want to collect data.”
Dr McDonald argues that: “We need all three in the room to make [electronic patient records] work. The problem is clinicians are often brought in too late.” Again, he says, this is where the CCIO role comes in.
Avoid the dark side
EHI ran the EHI CCIO Campaign last year to encourage all NHS organisations to consider appointing a CCIO. The CCIO Leaders Network has been set up to support the CCIOs that are already in place, and to make the case for others.
One of the debates that has raged since the campaign was established is whether CCIOs simply need a clinical background – or whether they should continue to do some clinical work.
Dr McDonald believes CCIOs should continue doing some clinical work to retain credibility and avoid being seen as “going to the dark side.”
Staying in a clinical role also means they have to use the systems being implemented themselves. “You won’t know it takes three hours to fill in a patient assessment if you don’t actually do it.”
Essential skills
The essential skills needed to be an effective CCIO in mental health are a discussion point as the psychiatrists break into workshop groups.
Attendees agree that a significant part of a psychiatrist’s skill set is being able to gather data and make sense of it, then communicate it in a meaningful way; in other words, to take a medical history, make a diagnosis and put in place a treatment plan.
As a result, they feel psychiatrists have a natural affinity with an information officer role. Technology can make a job harder or easier, but by engaging with IT, clinicians can work to ensure it is the latter.
One group thought some formal qualifications in change management would be helpful. But all agreed that a successful CCIO needs to understand the needs of all the different people using a system and to be able to communicate with different “tribes” within a trust.
They must also be able to relate to reality on the ground and understand the usability of systems and devices.
For example, one forensic psychiatrist relates how his IT department thought it would be a great idea to introduce tablets on to the wards – until he pointed out they would likely be smashed over a staff member’s head within minutes.
A common theme is that a CCIO should be able to admit something is wrong or not working properly, while still engendering hope that things can change.
The psychology of change
Towards the end of the day, Dr Jonathan Richardson, chair of the Royal College of Psychiatrists Informatics Committee, says there are already 18 clinical leads of informatics in mental health.
However, he believes leaders underestimate the difficulties of making people change at their peril. “There’s been a focus too much on technology, when you actually need to focus on the psychology of change,” he argues.
Dr Richardson is clinical director of informatics at Northumberland, Tyne and Wear NHS Foundation Trust, which has deployed a clinical dashboard.
Allowing staff to see how their performance compares with others has, in itself, bred changes in behaviour, he reveals.
A user defined summary of patient information – such as a dashboard – is one of the key achievements that one workshop group feels a CCIO should have managed within five years of taking up their post.
CCIOs should try for some “quick wins” in their first few years as “success breeds success”, one member says.
But other attendees push for more ambitious measurable goals; such as selecting a user-friendly central IT system for a trust.
More needed
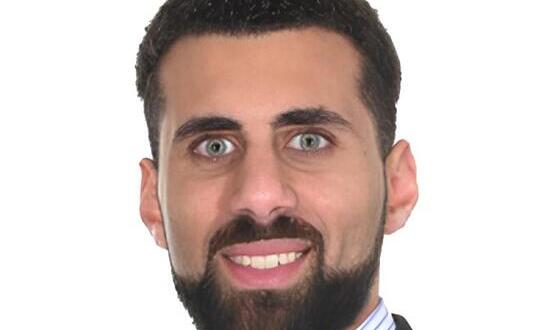
Dr Hashin Reza became clinical director of informatics at Oxleas NHS Foundation Trust last year – a CCIO in all but name.
He describes how his trust is doing a number of pilots involving digital pens and digital dictation, with results due in the autumn.
“Last year’s focus was to test and implement technologies that can reduce people’s dependence on the key board,” he says.
“From an organisational point of view, it did not make sense that very expensive highly skilled clinicians should be working as a typist.”
Dr Reza relies on clinical directorates to deliver projects, rather than taking ownership himself. He says the BCS group is a great example of the benefits of having a network of clinicians interested in IT and the CCIO Leaders Network expands on that.
“For me today was a very good thing,” he tells EHI after the event. “To be able to celebrate some of what’s been achieved so far and to see new faces in a room of people who are interested and enthusiastic is good, because we need more and more of them – the task is so huge.”
Notes from the event can be found in this PDF.