Hospitals to have e-records by 2014
- 22 January 2013

NHS hospitals will need to have operational electronic patient records working by April 2014 to meet the data flow requirements set by the NHS Commissioning Board and as a milestone towards making the NHS paperless by 2018.
Tim Kelsey, the NHS Commissioning Board’s mercurial director of patients and information, told eHealth Insider: “We’ve said that by April 2014 we are expecting a flow of data out of hospital electronic records, and this clearly implies trusts must have electronic records in place.”
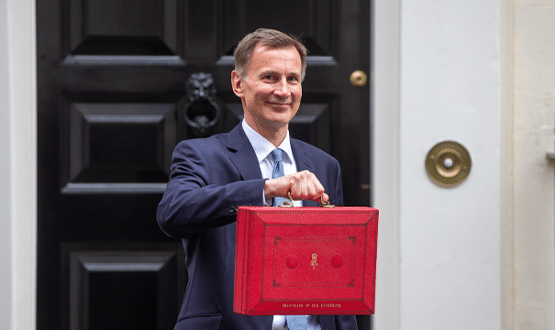
Health secretary Jeremy Hunt announced last week that he wanted electronic records and communications in place across health and social care by 2018 in a speech to the Policy Exchange think-tank.
In his presentation, he set out a number of milestones towards this goal, including getting electronic records into hospitals, making referrals paperless by 2015, and opening up GP records to patients by the same date.
However, the extremely ambitious new requirement on NHS providers was first flagged up in the NHS CB’s December’s planning guidance for the NHS, ‘Everyone Counts’.
Although the planning guidance focuses on data and its use rather than clinical systems – they get a mention on page 9 – Kelsey said electronic patient records “will be essential to enable the data flows required.”
The requirement for massive new flows of patient identifiable data, from hospital and GP systems, underpins the transparency, accountability and participation concepts at the heart of the NHS CB agenda.
Massive new flows of patient-level clinical data forms the basis for care.data, which will integrate health and social care data for commissioners.
New data will also be essential if the publication of consultant-level outcomes, to begin by summer 2013, is to be completed by 2014.
In primary care, where EPR systems are already in place, Kelsey says that the requirement for data to be automatically extracted from GP systems will be written into the replacement to the GP Systems of Choice Contract later this year.
Asked how the NHS CB could accelerate the adoption of EPRs, an area that NPfIT failed despite billions spent, he said: “We’re not in a position to put a massive investment into EPRs. I haven’t got hundreds of millions of pounds.”
However, he pointed to the success of the network of 60 US Regional Extension Centres in accelerating the adoption of EPRs and clinical IT as a highly successful model he’d like to try to emulate in the NHS.
He suggested that the spread of knowledge and know-how achieved by regional extension centres was a more important factor in accelerating EPR adoption than the $9 billion so far channeled through payments for ‘meaningful use’.
“The biggest change in adoption in the US came not from the meaningful use billions, but when [US President Barack] Obama set up Regional Extension Centers to train doctors and managers and develop and spread sustainable business models.”
Hunt’s vision will have to be achieved without central funding. However, in support of his speech, the DH issued a report from PriceWaterHouseCoopers suggesting that the NHS could save £4 billion by adopting new technology, including IT to make information available to clinicians at the point of care.
Kelsey said the NHS CB would invest in e-learning tools and in disseminating the available evidence base.
He also said a key part of the challenge is to get many more NHS clinicians and managers to ‘get’ that information and digital is “the biggest single answer to the QUIP challenge [to save £20 billion over four years to bridge the gap between flat funding and rising demand].”
The people who need to be won over he said, are not the e-health digerati and cognoscenti but those who remain to be convinced; "a hard-pressed GP working on the front-line in difficult circumstances, who sees all this as nonsense or a whimsical distraction.”
Read EHI editor Jon Hoeksma’s exclusive interview with Tim Kelsey in the Insight feature, The revolution will be digitised.