An NHS for the digital generation
- 30 May 2013

In the West, we have become used to improved living standards for the past fifty or more years. But there are concerns that the cost of healthcare is becoming unaffordable.
The NHS often defends itself against claims that it is inefficient by referring to international benchmarks against which it claims to represent value for money. However, the risk of benchmarking is that it gives a false sense of security and may simply compare one obsolescent system with one other.
Over the past decade, the NHS has absorbed massive increases in funding without increasing productivity. It now needs to find efficiency savings of between 4% and 6% a year to bridge the gap between constrained funding and the rising demand caused by rising medical costs and demographic changes.
However, constrained funds and fatter, older, sicker and better informed consumers are not the only challenges the NHS faces. Technology, medical advances and changed expectations will challenge it even further.
Information technology can save the NHS
It is clear that the NHS needs substantial changes to its working practices. But in the current context these can do little more than speed up a system at capacity.
Further, the NHS is essential a nine am to five pm service in a 24 hour world. This leaves expensive assets like operating theatres and imaging equipment under-utilised [and] is a mismatch with the expectations of the Digital Generation, who are used to service at their fingertips day and night.
At an abstract level, the NHS has three options: reduce demand; deal with demand more efficiently; and discharge patients quickly from expensive to less expensive care. A twenty-first century health system needs to address all three and effective IT can be a fundamental enabler of that.
IT can already help by reducing drug errors, promoting evidence based medicine, encouraging the development of structured medicine by enforcing care pathways, and enabling care to be delivered in cheaper settings, for example through telehealth and remote monitoring. However, the NHS has been slow to adopt these innovations. Why is this?
IT as a disruptor
In his book, ‘The Innovator’s Prescription’, Clayton Christensen says healthcare is mired in two delivery models: the large general hospital and the local doctor’s clinic. He also suggests that disruptive business models are created by new entrants to an industry, not by established institutions.
Established institutions can often develop a disruptive technology, but rarely do they combine it with a disruptive operational model. Often, when a disruptive technology appears, established practice disparages and rejects it.
Because it tends to simplify complicated problems, existing parties feel it cannot possibly address the complex problems they have been trained to address. Predictably, then, the reaction of NHS experts to IT has been mixed. When IT has been added to healthcare, it has been done without any thought of how the NHS could work better.
The goal of the National Programme for IT in the NHS was to create a cross-organisational patient record – perfect sense you might have thought – but the programme lacked an organisational vision. Benefits from technology arise from the human changes they underpin: computers buzz and humans do.
Uneasy past of the NHS and IT, and the limitations of Lean and other change methods
NPfIT’s problems have been exacerbated by other factors: it failed to get clinical engagement; most hospital boards have little or no IT expertise, and therefore fail to include technology in their planning; health informatics has been seen as something separate from healthcare.
But the essential problem was that it failed to learn the lessons of Professor Edith Mumford, who worked at Manchester Business School. She investigated the human and organisational effects of computer systems and showed that large computer projects often failed to produce the expected outcomes, even when the technology was sound – a phenomenon that became known as the ‘IT Productivity Paradox.’
Decades on, I still read research into healthcare that indicates that the lack of benefits arising from the implementation of IT is a surprise. It is not. Professor Mumford devised a design method named ETHICS – Effective Technical and Human Implementation of Computer-based Systems – to address this problem.
Professor Mumford’s approach has fallen from favour and fashion, but the underlying principle is sound: good systems design is far more than good technical design; it also requires a design approach that covers technology and the organisational context in which the technology is placed.
This implies the total redesign of departments, functions and areas, including roles, relationships, activities and jobs. There is some recognition of this. However, in recent years the implementation of IT has been associated with the use of methods such as Lean and Six Sigma; Lean to reduce waste and Six Sigma to reduce variability and defects.
Change managers have also had a bonanza, but without a burning platform as an incentive for the NHS to ‘jump in and swim’, the results have been modest. While the use of such methods is certainly a step in the right direction, most of the initiatives I have seen are mired in current thinking and lacking in radical innovation.
So, we end up by making obsolescent processes more efficient, instead of looking for new, more effective solutions. But reduced funding, changing epidemiology, and changed expectations are now fanning the flames licking the platform.
Vision of healthcare
Tomorrow’s healthcare is not today’s NHS. Tomorrow’s healthcare is integrated, continuous, standardised, personalised and based on evidence and prevention, rather than cure. The key is to escape from mindsets and to dare to create something new.
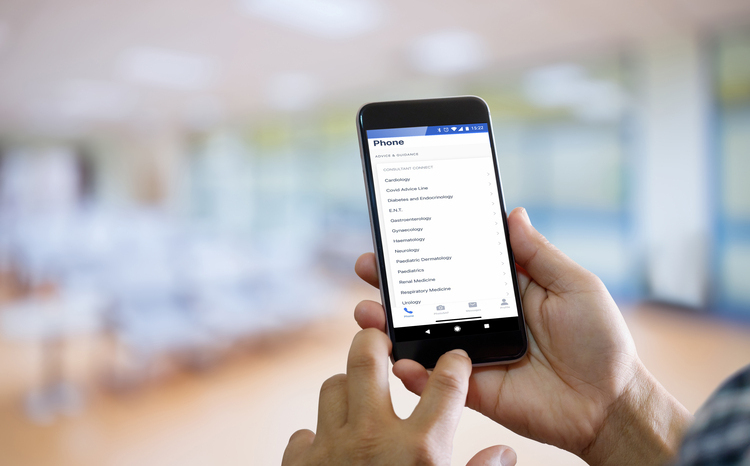
Future clinicians will have a comprehensive, continuous view of customers in real time. Remote monitoring can already monitor vital signs and warn of potential problems. In the future, convergence devices, like smartphones, will monitor vital signs, like heart rate, respiration, skin humidity. Through technology, the NHS’ founding aim of providing a cradle-to-grave service can be realised.
However, it will only be realised if it accepts organisational change, moving away from fixed locations and adopting technology to create new models of networked and virtual care, within which clinicians are supported by medical expertise encoded into software.
It will also mean a new relationship with patients, who will both expect care to be focused on their needs, and to take more responsibility for researching and managing their own conditions.
While I think about all this, I watch from my office window a girl of about six with her mother dragging her way to school, completely absorbed by a mobile phone. The Digital Generation has never known a world without computers, that’s why some call them screen babies.
Do you think the Digital Generation – let alone generation Y and even generation X – will accept the paper-fixated NHS? I mean, really?
Will people resist and get upset by the change I propose? Certainly. Creating a new system of care without upsetting someone is impossible. But, as Dr Johnson said, the prospect of being hanged focuses the mind wonderfully.
Part of me thinks the time is right for wholesale change, and part of me thinks powerful interests will make it impossible. To them, I say: please stop saving the NHS and start reinventing it.
Colin Jervis is an experienced consultant in healthcare transformation with IT. His book ‘Stop Saving the NHS and Start Reinventing It’ is available as both a paper and an e-book through the Amazon website.