Joe’s view of pushing rocks
- 28 August 2013
As usual at this time of year, you find me in the Eastern Mediterranean, sipping on raki and contemplating recent and ancient history.
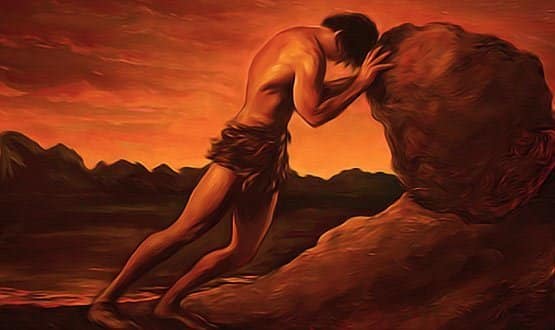
In particular I’m thinking about mythical king Sisyphus of this parish. I often feel Sisyphus should be the patron saint of NHS IT.
Sisyphus was the unfortunate king of what is now Corinth. He offended the Gods with his frequent pathological deceptions and as a punishment he was condemned to roll an enormous bolder up a steep hill – only to have it roll back to the bottom again on a daily basis.
Of Sisyphus’ dilemma Albert Camus said: “There can be no more dreadful punishment than futile and hopeless labor.”
Clinical engagement; everybody wants it
There’s nothing quite like a holiday to clear your mind, and I am finding that sunny climes are lending distance to the set of problems that beset me just before I left for the airport.
It’s nice to be popular, but as chair of the CCIO Leaders Network I am getting a lot of email asking for clinical input into NHS IT projects.
Sometimes the request is from NHS England, sometimes from the HSCIC, sometimes from the Department of Health, sometimes from Public Health England. And that’s just the national stuff.
I have also been invited to a variety of networking events for clinical commissioning groups and local area teams. And then there are professional bodies holding meetings where we could usefully have input; Royal Colleges, the PRSB, BCS, UKCHIP, the Faculty of Health Informatics… the list goes on.
It feels very much like the beginning of the national programme; people desperately trying to get sensible clinical input for big ticket, taxpayer-funded endeavours.
In a way that’s good, as we know these will fail without clinical engagement. The Summary Care Record is a technical triumph, but without clinical engagement it will wither and die.
The first rule of clinical engagement
Still, clinical engagement is more than having a few clinicians, however excellent and committed, hired to work on the project.
It’s having a big enough group of credible clinicians who get heard when they say: “SCR? I don’t use it because there’s nothing in it” and: “Why can’t I add a care plan?”
As such, the road to failed clinical engagement is paved with good intentions. A good example was the recent round of applications to the £260m Technology Fund, organised by NHS England.
I was delighted to be asked to be a judge, but with two weeks’ notice I couldn’t possibly get involved without cancelling clinics.
I know that it’s difficult to explain the practicalities to politicians when they set impossible timeframes, but explain them we must. So, the first rule of clinical engagement is that real clinicians need eight weeks’ notice.
Two more rules of clinical engagement
I learned some crucial lessons about clinical engagement when I worked on NPfIT.
One is that if a different set of clinicians turns up for every meeting you will spend 70% of your meeting justifying what absent clinicians said at the last meeting and the other 30% trying to explain to the newcomers what it is you want them to do.
So the second rule of clinical engagement is to make sure that you keep getting the same bunch of people in the room.
Finally, when I studied medicine nurses trained for three years and you could tell the stage of their training by their hats – one stripe = 1st year student, two stripes = 2nd year student, three stripes = 3rd year student.
This was very helpful because, at a glance, you had some idea of how much knowledge to expect of a person.
Sadly, clinicians are not similarly striped with regard to their understanding of health IT, so the quality of their input can only be assessed as you get to know them during the engagement activity.
This means that to be effective, there are three rules for clinical engagement. The activity needs to be timely (enough notice), consistent (not a different set of clinicians every week) and knowledgable (about e-health, or everybody will spend hours educating each other).
In addition, clinical expertise needs to be independent of both government and system suppliers and therefore free of the conflicts of interest that proved so damaging during NPfIT.
At the moment, despite all the invitations (and once again thank you, we do appreciate being asked) I feel we have launched a new National Programme for IT in the NHS.
We could call it NPfIT II; a big goal of paperless by 2018 with a new version of NHSmail, with a different dataset for every clinical commissioning group, and data for Francis, data for Keogh, data for Berwick, data for Monitor, data for CQC, data for PHE, and data for anybody else with a report out.
Unfortunately, the current clinical engagement arrangements are actually worse than those put in place by NHS Connecting for Health, which at least realised that clinical engagement was needed, even if it got there at little too late to succeed.
Given that there isn’t the money this time around to hire dedicated clinicians to support all this work, another way will have to be found.
A clinical IT engagement strategy will need to be produced and in order for it not to be produced in triplicate someone will have to decide ‘who is the clinical informatics engagement daddy?’ The DH, HSCIC, NHS England or Public Health England?
Time for NHS England to take charge
For me it should be NHS England. NHS England has the money and therefore the clout to make the necessary strategy happen. So here’s a suggested clinical engagement strategy for NHS England:
- NHS England will not deal with any organisation that does not have a chief clinical information officer by April 2014
- It is a part of the CCIO’s role to support national programmes
- NHS England will financially support existing clinical networks rather declare ‘year zero’ and attempt to impose a top down solution.
I can’t speak for primary care – and frankly primary care people are pretty good at speaking for themselves – but in secondary care we have an urgent need to develop a cadre of CCIOs to form the vanguard of the information revolution.
It is a requirement for every trust to have a senior clinician for child protection and for infection control and for information governance, so surely it is time to mandate a CCIO for every trust?
Now, I would say that wouldn’t I? Well yes, I suppose you’re right; but if you’ve got a better idea please put it in the comments section below.
Act now to avoid Sisyphus’ fate
I do feel that we need to act quickly or risk sharing Sisyphus’ fate. In a final deception, the king of Corinth told his wife to bury him without the requisite gold coin in his mouth.
The idea was that he would have no money to pay the ferryman to carry him across the river Styx to the underworld. With no money to pay the ferryman, Sisyphus hoped to avoid crossing the river and so to cheat death.
Instead, he condemned himself to endlessly repeated failure. We need to collectively roll the clinical engagement boulder up to the top of the hill and, using just enough gold, wedge it firmly and permanently in the sunny uplands.
The CCIO Leaders Network is answering as many requests as we can for clinical input at the moment; but we can only provide a limited service until someone pays the ferryman.
The second annual CCIO Leaders Network will be taking place alongside EHI Live 2013 at the NEC in Birmingham in November. Dr Joe McDonald will also be speaking at the fourth annual meeting of the National Mental Health Informatics Network, which is coming to Live for the first time. EHI Live 2013 is a two day conference and exhibition at the NEC in Birmingham on 5-6 November. This year, the conference is free for all visitors, and registration is open now.




