Royal College of Pathologists appointing lead for diagnostic digital pathology
- 20 September 2017

The Royal College of Pathologists is recruiting a clinical lead for diagnostic digital pathology, following its publication of a strategy suggesting the technology offers potential efficiency and quality benefits.
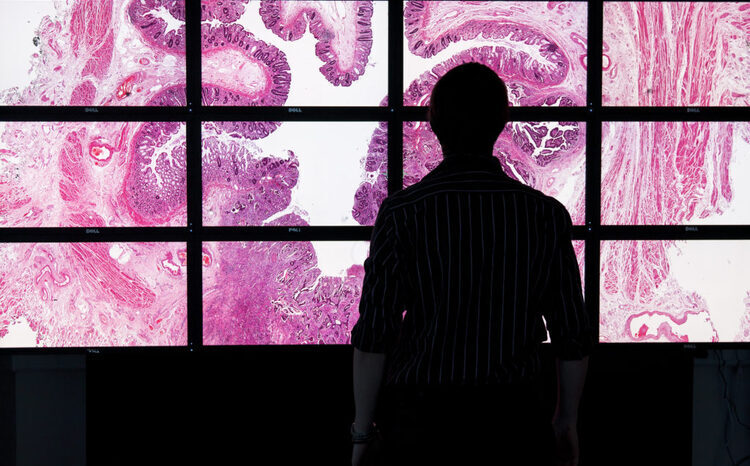
The document is the first time the College has formally published a strategy on diagnostic digital pathology, which involves scanning glass slides and viewing them via a computer rather than down a microscope.
The author of the strategy, which was published last month, told Digital Health News he felt RCPath was now “happy to encourage laboratories and groups of laboratories to develop digital services”.
Professor Tim Helliwell, who is consultant histopathologist at Liverpool Clinical Laboratories and the College’s vice-president for learning, added: “I think the College is hoping that, over the next five years or so, there is a gradual transition from a predominantly microscope-based pattern of service delivery to a computer-based digital mechanism of service delivery.”
The new clinical lead for diagnostic digital pathology would, it is envisaged, support this change. Applications for the role close at the end of this week.
The advertisement says the successful candidate “will play a key role in advising laboratories in the use of digital pathology for diagnostic use and will work with others in the College to advise on how digital pathology should be included in curricula to support the training and assessment of future pathologists”.
Both the strategy and the new post can be seen as a significant evolution in the College’s attitude to digital pathology for diagnostic use.
As recently as November 2016, RCPath president Suzy Lishman told Digital Health News there was “not yet sufficient evidence to support its wholesale adoption”.
Helliwell did stress that going digital is “not the solution for everything; not the solution for every laboratory” and that it can be time consuming to implement.
But he said a number of developments over the past 12 months had now given the College “confidence that we can make recommendations”.
He said those developments included improvements in the quality of suppliers’ products, a growing body of research suggesting the technology is safe to use, and the US Food and Drug Administration’s approval of a Phillips’ digital pathology solution.
That approval, granted in April, represents the first time the US regulatory body approved such a solution for primary diagnostic use.
Proponents of digital pathology argue that it will enable staff to work more flexibly – including from home – and to more effectively spread workloads.
There is also hope that artificial intelligence could ultimately help pathologists interpret images, and so make better diagnoses.
Last month, the Life Sciences Industrial Strategy suggested that “systematic digitisation of pathology images could be readily established providing substantial efficiencies in the pathology service within the NHS, allowing the system to become increasingly virtual and reducing the need for every hospital to have the full on-site set of pathologists”.
While the life sciences strategy constitutes recommends to the government rather than formal policy, Simon Stevens has indicated NHS England is backing its recommendations.