DrDoctor to be trialled across 11 more NHS hospitals
- 23 October 2018
Online tool DrDoctor is to be trialled across more NHS hospitals in England.
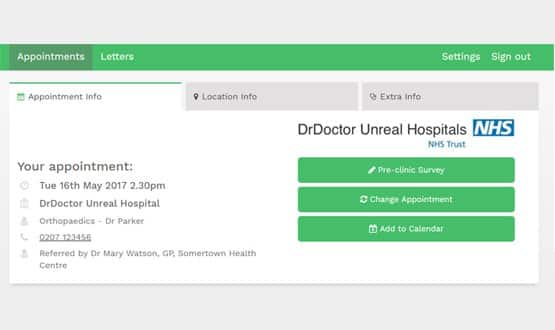
The technology allows patients to book and change medical appointments online, receive text reminders and provides access to maps to guide patients to the right department in hospital.
Patients can also fill in medical forms before they arrive and receive appointment letters digitally via the platform.
DrDoctor is already used in ten hospitals, including Guy’s and St Thomas’ NHS Foundation Trust and Frimley Health NHS Trust. It will soon be trialled in 11 more across the country.
These NHS sites have been specially selected to test the impact of DrDoctor across a variety of hospitals, from small specialist sites to large inner-city establishments, with plans to begin the pilot by March.
Simon Stevens, chief executive of NHS England, said: “As the NHS develops its long term plan we will be looking to new technology to drive improvements in patient care and improve our efficiency.
“This technology has the potential to be a triple win for the NHS by making life easier for patients, saving money and improving appointment efficiency.”
NHS England suggests that DrDoctor can save each hospital £2m a year by reducing the number of missed appointments and cutting down on postage costs.
DrDoctor was part of DigitalHealth.London’s accelerator programme, which aims to speed up the adoption of technology in London’s NHS by working with start-ups and SMEs toward solutions that address the most pressing challenges facing the health service.
Sam Roberts, director of innovation and life sciences at NHS England, said: “The NHS is always open to new technologies and today we have put our money behind our intentions by directly funding these tools.
“Promising innovations often struggle to gather the evidence they need to enable their rollout in the NHS, which is why it so important we have programmes like this to allow us to gather the evidence we need to help spread the use of new technologies that can save money and improve care for patients.”
In April, DrDoctor partnered up with Intouch with Health to deliver an outpatient portal that can be integrated with trust PASs.





15 Comments
Sorry I am trying to understand the concept/difference between DrDoctor and the eRS service. Can somebody explain this?
Can the eRS system not integrate in to whatever DrDoctor are trying to achieve?
Indeed, so am I. Surely, text reminders, digital appointment letters and maps should just be (long-overdue) add-ons to ERS, not a brand new system, – probably incompatible with ERS.
And, “DrDoctor” is a jolly silly name.
In all, a typical bit of NHS wonky digital planning.
Technology that has been used in primary care for many years. Hardly high tech and ridiculous assement of money saved – ie cash released from NHSE.
I think most posters are missing the point of this application. This is about appointments, not referrals, for which ERS is mandated (and if you are not allowing patients to book real appointments but you are still using CAS clinics and contacting the patient, you haven’t implemented ERS properly!). The processes are in fact very clear, and yes there is a real problem with Outpatient capacity being wasted by DNAs.
Once a patient has an appointment booked, whether new (after ERS referral/triage/booking) or follow-up (however booked) , they can be sent a reminder by SMS just before the appointment date. This allows them to cancel and rebook if they choose. This significantly reduces DNA rates , eliminates phone calls and offers a much better patient experience. This principle can also be applied to pre-assessment and TCI bookings. Integration with PAS is very simple. What’s not to like?
Yet again an example of technology trying to solve a problem without clear understanding of what the processes involved are and if a real problem exists.
To a certain extent, I agree, but technology can help drive process discussions, at least. (whether or not that happens, the jury is out.)
Intouch with health’s kiosks are an interesting technology (which I thought could be revolutionary) that actually proves your point, though. To understand the use of kiosks in hospitals, I sat in one for a number of hours watching their use – I don’t know exactly how much they cost the hospital, but not a single machine was used in that time. With patients preferring to wait at the reception desk for the next available real person.
Missed appointments are costly, so any effort to reduce those is positive, but I worry that some of that saving will be offset by future technology costs (integrating with DrDoctor, for example, because it’s not really considered the wider picture). But because the system is simple, this may not be an issue.
The processes are very clear, as are the different roles of ERS, PAS and Dr Doctor.
ERS allows GPs to refer patients to the Acute Hospital. It also allows the patient to book an appointment. The referrals are then triaged by the consultant using ERS.
DR Doctor is attached to the Acute Hospital patient administration system and receives notifications of forthcoming appointments. It will send a text reminder to the patient just prior to the appointment. The patient can then cancel and rebook.
If the patient is given a follow-up appointment at the hospital, Dr Doctor will also be notified and will send a timely reminder to the patient. They then have the same option to cancel and rebook.
ERS does not have the ability to contact the patient in this way – that is not its purpose. It is the Hospital Patient Administration System which must record whether a) the patient opts to be contactable by text and b) their mobile phone number.
The savings are real in terms of reduction in DNA’s (which waste outpatient capacity and can impact patient outcomes).
As someone who sounds like they may be involved in the project, how do you get around different PAS requirements for integration?
Or does DrDoctor actually use a messaging standard (HL7 I would assume with the PASs generally in use), or are these 11 hospitals all using the same PAS, and that’s why they’ve been selected?
Well, eRS means patients generally book the time and place of their first out patient appointment themselves, online or via a booking office.
Being able to amend the follow-up appointments in this way would be useful, no doubt.
It can either use HL7 standard messaging or sql query on a data warehouse table to get patient and appointment data. Either way very easy to set up.
How does it get around data ownership though? If it’s not a system deployed locally, then there are serious GDPR concerns around who is responsible for the data.
Giving DrDoctor access to a database already sounds like a terrible idea, because many healthcare providers , and their DBAs (if they have any), don’t really manage security very well. HL7 allows a bit more control, but from what I have seen of HL7 integration is that there isn’t enough expertise in the industry to understand the impact of what their systems send to third parties.
Interoperability in healthcare is a really back-to-front model that is keeping the industry in the status quo – my worry is that these ‘innovative’ companies are just looking to take what they can from the industry and achieve an exit for their investors – this isn’t necessarily a bad thing, but they’re not changing the sector for the better on their journey.
But perhaps this is just the healthcare sector, and DrDoctor, having grown out of an NHS trust, is just servicing an immediate need because there isn’t the insight in the industry to truly understand how technology could do so much more than improve the booking experience with little extra effort.
Sorry, that moan came out of a talk about HL7, which, while an aging standard, has got a number of benefits, and the industry couldn’t run without it, but HL7, and even FHIR are solutions to problems that are legacy problems, and the healthtech sector should be making those problems irrelevant rather than continue to service them.
I am confused by the cpmments from Dr Neil Bhatia, and Jono. My understanding is that once a GP has referred a patient, the hospital booking department would contact the patient to book their own appointment at a time they choose. Similarly, patients with follow up appointments (usually booked at end of an appointment) would be able to alter the day or time if needed.
I would welcome such a system, as an alternative to long waits on the phone to speak to someone to alter or book appointments. Ditto the online firm filling, with the patient having the option to fill in forms at home rather than struggle to write or recall details in the waiting area.
Yes, changing appointments once booked is valuable – it should help to prevent no-shows. I’m not aware of the referral process being part of DrDoctor though, so there’s no value add from the software there (at least, not yet).
Still, I haven’t seen how comprehensive the InTouch with health portal is. Maybe some of that process is covered there.
Follow ups for a single episode are often booked one at a time, but people with recurring or long term illnesses have a much harder go of it. And perhaps that’s a problem the NHS has in general – 13 weeks between small appointments is just wasting resources; but that not DrDoctor’s fault, and maybe they can help change it in the future.
I welcome innovation, but an appointment booking system is the low hanging fruit. Hospital systems are so much more complex than appointments. With it being born out of Thomas and Guys, I guess there is a real need for it in the NHS though!
I’m confused.
Presumably this is out with the booking mechanism for 1st specialist appointments, following an eRS by the GP?
So is this for all other appointments, follow-ups etc?
I don’t even think follow ups – more for GPs I would assume.
There’s no triage capability, and it would be hard to gauge a follow up without some understanding of hospital process to know where one episode ends and another begins.
It’s something my own company has been working on in the private space, and we’re starting from the integration out, rather than appointments being central to the system (using an order-oriented workflow).
It’s an interesting challenge, and I worry that DrDoctor, while a great piece of software, might be adding further technical debt to the hospitals.
Comments are closed.