Orion labels 2018 ‘key year’ at annual customer conference
- 21 November 2018
Orion Health underlined its commitment to driving forward interoperability in the UK and Ireland during its annual customer conference in Birmingham.
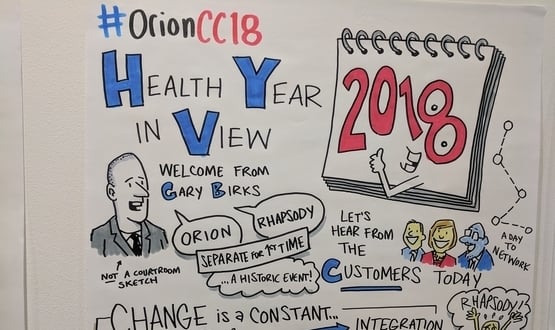
Addressing delegates on 6 and 7 November, representatives from Orion Health offered updates on ongoing projects and outlined the future ambitions, in what was described as a “key year” for the supplier.
Gary Birks, Orion Health’s general manager for UK and Ireland, alluded to tricky times faced by the company in 2018, which saw its core integration business sold off to a British investment firm.
In an opening address to delegates, Birks said: “This is quite a historical customer conference for Orion – for the first time, Orion and Rhapsody exist as two separate organisations.
“We’ve gone through significant change and it’s only right to recognise that tech companies in healthcare can expect to go through change all the time. It’s a constant for us and it is why we love to work in this industry.”
Orion sold off Rhapsody, the company’s software integration engine, to private investment firm Hg this year after posting losses of NZD $40m (£20.9m).
Company CEO Ian McCrae suggested that waning income from the US – which constitutes around half of Orion’s total income – was to blame.
McCrae explained that US customers had started running out of money just as the New Zealand-based supplier had begun pouring resources into the cloud, labelling it “the perfect storm”.
“Half our market entrenched when we were doubling down on R&D – it was very unhelpful,” offered McCrae.
Pushing the interoperability agenda
Elsewhere at the two-day conference, Orion provided attendees with updates on ongoing pieces of work.
This included Bristol’s shared record project, Connecting Care, where authorities have started using FHIR APIS for controlled drug prescriptions.
The API was developed to cut substance abuse by reducing the risk of duplicate prescriptions being issued for the same person.
Emlyn Jones, the programme’s technical lead for interoperability, praised the speed at which the project had been rolled out, taking as little as five weeks from approaching the supplier to being ready to go live.
Jones credited this to the platform’s use of a standard interface, despite having to convince the supplier of Bristol City Council’s Theseus substance abuse platform to use FHIR APIs.
“These standards aren’t finished or completely mature and some suppliers won’t want to use them as they are,” he said.
“But they won’t get finished until we use them, and we ask suppliers to use these interfaces and feed them back.”
“Whether we think FHIR is the right standard, it is definitely going to be used within the NHS.
“The only way to find out is to try it.”
Varying landscapes
Jones’ sentiment was echoed by Dougal Fleming, technical services manager for Orion Health, who outlined differences in the interoperability landscapes of England, Scotland and Northern Ireland.
Fleming suggested that Northern Ireland in particular boasted “an excellent level of integration across systems” – partly owing to the small size of the country, which by default made issues “more manageable”. He also said there were “good examples of reuse” of successful work, resulting in a lower level of fragmentation and less time spent trying to do things from scratch.
Work had also proved “ahead of its time” in Scotland, Fleming suggested, thanks to “pretty good national systems” and large programmes of work around information sharing between health boards.
As for England, despite a number of shared care record projects currently underway, Fleming cited challenges around collaboration between regions and differentiating interfaces and the quality and consistency of data being collected.
He also argued the use of data was “not necessarily thought through” and “only sufficient in scope to fulfil the needs of that individual system”, rather than wider populations.
“It takes significant time, effort and money until you have a critical mass of useful information to drive benefit out of the system from,” said Fleming.
“We are effectively reinventing the wheel each time, because the system as it exists at the moment has very little integration in it, and there is little obligation on systems to release data in a usable form.
“We need to change this. We don’t know what will have the biggest impact, but we can be fairly safe in understanding that the foundations for predictive and proactive care are going to lie in integration and interoperability.
“As an industry, we are collectively underachieving on both counts.”
Patients as a vector
Orion also used the event to promote its new machine learning service, Amadeus Intelligence, which it hopes to position as a key clinical support tool within health and social care in the UK and Ireland.
The firm has developed a research methodology for combining clinical data sets to represent patients as “a mathematical vector”. Kevin Ross, head of machine learning at Orion Health, explained this made it easier for machine learning algorithms to match patients with similar individuals, and spot patterns in symptoms and health outcomes.
Anne O’Hanlon, product director of Amadeus Intelligence, suggested there was a need to “guide algorithms so they think more like humans”.
While she acknowledged there was a “lot of hype” about machine learning – not to mention a tangle of regulatory issues yet to be hammered out – there was also “tangible clinical value and savings to be realised”.
“On the ground I’m seeing there are a lot of people asking: ‘How do we make it work right now when the data quality isn’t there yet?’” said O’Hanlon.
“Cloud and computing power is driving change. Legislation and regulation will catch up.”




