NW London Care Information Exchange begins mass recruitment
- 4 December 2018

Residents of North West London are set to benefit from being part of one of the largest shared patient portal programs in the UK, with mass registrations now underway.
The Care Information Exchange (CIE) hosts the health records of up to 2.3 million people living in North West London, and is using an open platform with APIs to enable sharing across London and other parts of the UK.
Some 50,000 patients in north west London are currently being invited with over 10,000 already signed up. So far 20% of patients invited to register are signing up, with the number rising to 90% if they have test results on the system.
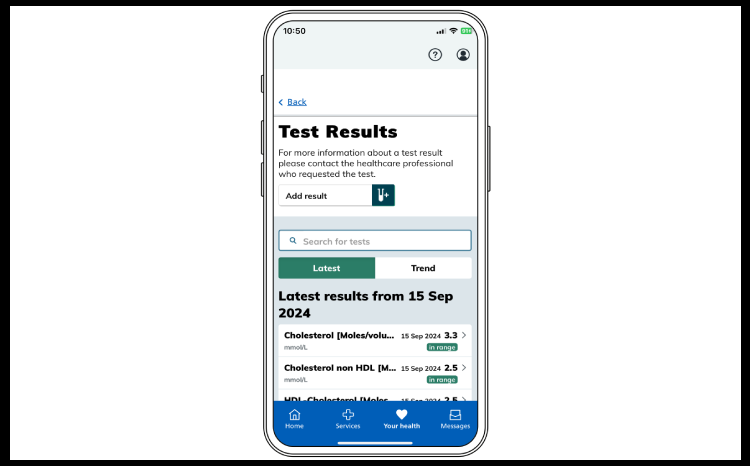
Powered by patient-controlled personal health record (PHR) specialist Patients Know Best, and funded by £3 million investment from Imperial Health Charity, CIE collects data from hospitals and GP practices in the area. It also connects to 15 other hospitals outside of north west London including Birmingham, Bristol, Liverpool, Manchester, Scotland and Wales.
While most hospital or GP portals tie the patient to a single institution, PKB claims CIE offers a true patient portal, enabling patients to access their health record from anywhere in the world and share it with any institution, professional or carer wherever they are.
The CIE system uses Application Programming Interfaces (APIs) to display data in context within local medical systems. The system enables hospital clinicians to see data about their patients who may also have been treated elsewhere in the country.
With the introduction of mass registration, people can now sign up to access their health record at scale and with speed in a number of ways; either by speaking to a member of staff; by using the kiosk check-in screen commonly found in waiting rooms during their outpatient appointment; or by letter of invitation to their home.
Imperial College Healthcare NHS Trust found automated kiosk registrations led to over 3,000 patients in the first month alone with more than 70 people completing registration every day.
Kevin Jarrold, CIO at Imperial College Healthcare NHS Trust and Chelsea & Westminster NHS Foundation Trust, added: “We designed CIE so the data follows the patient wherever they are in the UK or rest of the world.”
He added: “It was important for us to choose a patient portal that allows patients to share data with any provider, and with open read-write APIs to integrate with their systems.”
Andy Kinnear, CIO of the Connecting Care shared record programme in Bristol, said the model allows patients who travel between Bristol and North West London for tertiary care to easily share their data.
He said: “It’s great that all data is truly available to the NHS via open APIs. But more than that, there is a consent layer that allows patients to express their preference on being contacted, taking part in research and sharing with friends and family that actually care for them. We have already had professionals in Bristol access data from London, and vice-versa.”
Dr Mohammad Al-Ubaydli, founder & CEO of Patients Know Best, told Digital Health News, “Institutions funding this in the UK are doing this because of the cash savings from patients logging in to view their test result data or make an appointment .”
“In Surrey [another PKB customer] we’ve helped the trust save £4m through saved appointments by patients logging in and looking at test results instead of coming in for an appointment,” he added
“So it’s enabling the clinical transformation of patients not needing an appointment of coming into A&E in the first place, that is where the real financial and patient benefits of digital channel shift occur.”
The PKB consent model places the patient in charge of deciding who they want to share their information with.
So far, more than 10,000 patients have registered with CIE and 31% have also consented to share data for research purposes.



23 Comments
I have done my share of health IT, which is why I follow these discussions. But I am also a patient, and being a patient is extremely hard work. Checking appointments. Test results in one hospital system (via GP) when outpatient visits are at another (tertiary service). And a hospital which decided to microfilm all the most important parts of my record when they changed PAS.
I am registered on Care Information Exchange (aka Patients Know Best). Some of the comments above about consent are wrong. While data will be loaded from source systems to CIE, nobody ( and I mean that) can see it (1) until the patient chooses to register (in which case the patient can see their own data), and then (2) until the patient offers a share (with content selectivity) to their clinical team(s). Those shares can be modified or cancelled at any time.
I would agree that test results may need some explaining, and there are many information sources available to help with that. Clinical correspondence copies are useful too. But the real use of these and others is proof that they have happened. How much time do patients waste wondering if anyone has actioned a request or referral.
CIE can recruit as many patients as it likes, but what I really look forward to is recruitment of many more data sources (hospitals and especially GPs). At the moment I can see my data from one place, but not from anywhere else.
I found the developer specs for PKB (wow, big plus from me on having them public).
I can see what is behind this, so I withdraw some of my comments. The ability for patients to see correspondence and summary of medical encounters looks like a great service.
It does have some old school tech but that’s a practical level.
I’m getting a little confused by this PHR terminology.
My recent health data is held on a number of cloud servers. How does these openEHR or PKB servers fit in with this?
My main concern is this seems to be implying I’d want to move my data to a central store (sorry no it’s staying where it is – nhs can access if they are giving me care).
Their are also no tech reasons why my phr needs central storage (ok for some apple data it needs moving but for most that’s not true)
I have an issue with the fact data is uploaded even if you don’t want data uploaded, and your sharing preferences are set to not share. There is no need for central data storage. The obvious answer is explicit consent for GP data to be uploaded, and data from other organisations will only be uploaded if you already have had GP data uploaded. Otherwise patients think they have fully opted-out, without realising their data is still being uploaded.
Things need to be consensual and fully transparent if the NHS wants patients’ trust.
This seems to be legacy system design. Let’s call it let’s call it openNPFIT.
If a phr needs data it doesn’t hold it goes and gets it.
It doesn’t need a central database and ye old messaging like digital child health.
It also says 31% of patients have consented to the use of their data for research. Is this proper consent, or NHS defined consent? Because the NHS has a different definition for consent than the rest of society.
There is a danger that data uploaded from different organisations to one location will be used for purposes other than which the data subject has consented or has knowledge of. The NHS will claim that this data is ‘anonymised’, because again the NHS uses a different definition of the word ‘anonymous’ than the rest of society. But it isn’t anonymous, because its been accumulated from different sources by the use of a consistent identifier.
It doesn’t help to guess what CIE does or doesn’t do. The CIE site has all the real explanations of its functionality, including around consent. Essentially, a research team can be added as a share in various ways, including by the patient actively registering via the team. Anyway, all shares can be viewed by the patient at any time and the patient can edit (by categories) or cancel a share at their absolute discretion. It really is the case that the patient is in complete control. ‘Patient Knows Best’ is not just a slogan: it’s the basis of the system. At last we have something where the patient has ownership.
Agree but also I should have to reverse engineer descriptions to work out what it is doing.
I’m seeing year 2000 tech, it’s a central database which implies it’s security is old.
Mention restful api, oauth2 (Openid and authorisation). I start to get happy the managers of this know what they are doing.
What we want is a co-produced PHR – Ecosystem as described in this document just published by the Apperta Foundation.
https://apperta.org/coPHR/
We are already talking to openPHR and it would be great for PKB to join us in creating a truly open ecosystem that put the patient at the heart of care.
I can see that. The user requirements in co-phr are quite good, PKB compliments that with technical specs. Their is a gap in both on processes involved (I can infer what they are in PKB).
Ewan – while I appreciate what Apperta has done – they represent a handful of very intelligent individuals. The Apperta document is by no means an international definition of open standards. Surely we cannot define such an internationally used term across industries by this paper?
The vast majority of people would agree with this from Wikipedia (appreciate, this is not the foundation of all knowledge, but referenced from a Harvard Business School):
In computing, an open platform describes a software system which is based on open standards, such as published and fully documented external application programming interfaces (API) that allow using the software to function in other ways than the original programmer intended, without requiring modification of the source code. Using these interfaces, a third party could integrate with the platform to add functionality.[1] The opposite is a closed platform.
Many current “proprietary” applications offer API’s as above – therefore – open platforms.
Excellent just get on and deliver it across the UK and stop local STP’s trying to create something from nothing . Need this in Kent and Medway ….Now! (Annoyed patient relative)
While I welcome this initiative let’s be clear this is not an open platform. It’s PKB’s proprietary platform with some open APIs.
An open platform requires that there is no vendor lock-in and that data is stored in a open transportable format.
see openplatforms.apperta.org
You probably know I’m an advocate of open platforms, but we should ask ourselves, is this really want the patient wants? Surely they don’t care what format the data is in as long as it’s accurate, complete, within their control and widely accessible?
They might only care if/when they want to move their data from one PHR to another and are told it isn’t possible or not everything will be transferred.
Hi Ewan
I think we disagree over definitions of open platforms.
So I thought I would spell out the individual facts:
1. PKB data storage is proprietary
2. PKB source code is proprietary
3. Every data point we store is available with a read-write open REST API – we have made this available from the beginning on http://dev.patientsknowbest.com with OAuth for authentication and consent
4. In 2018 we started to migrate our proprietary syntax REST APIs to open standard FHIR ones and intend to complete this in 2019. These FHIR are the APIs we use for our own source code as well as being open for anyone else.
It’s based on (3) and (4) that we say PKB is an open platform.
Even if your definition is based on all of (1) to (4), every PKB customer is able to use our APIs with their preferred systems for all the data held in PKB. There is no vendor lock-in. One of the reasons customers like us is they can leave us if they don’t like us anymore. And meanwhile their patients can receive data from any other party and share data with anyone they want.
And that’s what NWL have achieved for their patients open to providers across the world and already receiving data from across the U.K..
okay, that is positive, but lots of test results need interpretation by a qualified physician so best to keep what’s displayed simple !
Thanks Clive take a look at this video of a patient speaking about using the system:
https://vimeo.com/285905475
She can understand most of the results already because we include explanations designed for patients.
But she also has time to prepare her questions in advance of her appointments. Without PKB she would not have time to take in all the information during the appointment and would only think of questions to ask after the appointment finished. And then it’s too late. Seeing the data in advance is much better for the patient and it’s also a much better use of the clinician’s time with the patient.
The BBC are the world leader in health communication. The key words for me were NATIONAL approach. I have a NATIONAL DATA model that supports the Unique Health Journey, based on a person’s pathways (a person’s results should be filed against a specific pathway). Please let me have a better way of contacting Mohammad so that I may share, my name is Clive Spindley and I work at CUH NHS FT. Thank You.
I totally agree Mohammad. All contracts I have seen, have the vendors on the hook to transfer data to another platform at the end of the contract – therefore – no lock in.
Personally as a patient, I would much prefer a system that works. Whether proprietary or not, however I have greater piece of mind with the proprietary side of things.
As open standards are really beginning to enter the limelight, the perceived benefit of Open Source is going away. Proprietary platforms are allowing clients to innovate within the platform – meeting the need that Open Source originally met.
Some of the biggest Open Source projects are moving to proprietary.
My metaphor – doctors should be asked how to design the new wing of the hospital, not get a spade out – however should they want to paint a wall they can. Anyone feel free to use that
I’ll use that!
Open platforms are not about open source – You can build a open platform with entirely proprietary components. Indeed the market leading real-world implementations rely on proprietary components. .
You can also build with an entirely open-source stack. Open or closed source is not the issue here and I really don’t care and recognise the difficulty of creating economically sustainable open source business models in health.
I don’t agree that most contract have meaningful requirements to transfer data to another system. A few do many don’t. I don’t know about the specifics here Mo may wish to comment.
OK Mo but you don’t meet the 8 principle in the Apperta document Defining an open Platform.
A question. Is your API open IPR. i.e if I wanted to replicate your API on (say) an openEHR Clinical Data Repository such that it could replace the PKB data store without disturbing the applications running on could I do this without permission from or payment to PKB or any one else. If Yes can you point to your API definition on GitHub (or similar open repository) and tell me the licence under which you make it available.
If your answer is yes then I might concede you meet much of the spirit of an open platform (if not the letter of the Apperta document)
If no then it’s a proprietary platform
“Is your API open IPR.”
Oh that’s a clever question, I like that. Apologies I had misunderstood your original point about open platforms.
Short answer “no”.
Long answer “no because we assumed people would prefer we switched our APIs to open standard ones like FHIR rather them than learning APIs we had come up with.”
The biggest gaps we found in FHIR so far are care plans and privacy labels. Again our focus is on working with the FHIR community to expand their APIs which we then use internally rather than having others learn our APIs.
I like that Apperta is open sourcing the IPR for its APIs. Right now if I show our FHIR adoption to CIOs they get it and like it but I think I would have to explain Apperta to them. (As you had to explain to me.)
Comments are closed.