The idea of the NHS offering more options for remote consultation and more care outside hospitals is far from a new one. But with Covid it’s taken on a real urgency and led to new demand for vendors working in the sphere. In the first of our Industry Spotlight series, Claire Read speaks to Jonathan Patrick of Consultant Connect about the practicalities of a vendor managing this explosion in interest – and what comes next.
Jonathan Patrick had been used to presiding over a healthcare tech company experiencing steady growth. As chief executive of Consultant Connect he has led a firm which, following its first project in June 2015, had grown to cover 50 or 60 hospitals by January 2020.
Then Covid hit. With it came an explosion in interest which Patrick says the term ‘uptick’ fails to adequately characterise.
“It’s been the most astonishing period of growth in both usage and in terms of our footprint around the country. It took us four and a half years to get to where we were at the beginning of the year, and then in the following four months we achieved the same amount of growth again.”
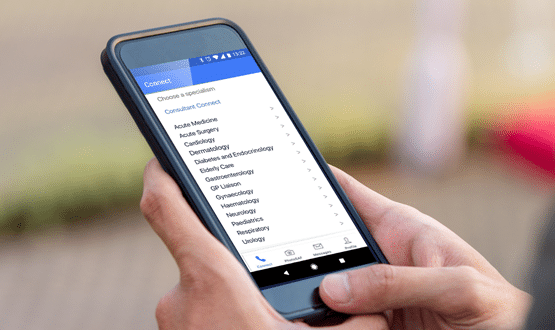
The company provides services enabling clinicians to easily seek clinical decision support from colleagues. Initially that meant GPs able to contact secondary care doctors, but it now also means supporting paramedics to connect to GPs and specialists to understand whether a patient needs to be taken to hospital or could be cared for within primary care.
The idea is that, through straightforward access to advice – a rota system means doctors only take calls when they are available and, if one person is unable to answer a call, it goes to the next person on the list – inappropriate hospital referrals and attendances can be avoided.
In areas particularly badly affected by Covid, calls from GPs to specialists via Consultant Connect to seek advice about a patient have avoided hospital referrals in as much as 90% of cases.
In other words, it’s a service perfectly suited to fulfilling the NHS’s new mantra of ‘talk before you walk’, in which the default is for patients to be consulted and counselled remotely before any in-person appointment – so reducing potential exposure to coronavirus.
“The importance of communications networks between patients and GPs, GPs and secondary care and secondary care to primary care has suddenly just rocketed,” reports Patrick.
Understandably, so too has the speed with which NHS organisations expect private vendors to implement solutions (“commissioners were expediting their commissioning decisions, and as a consequence there was a firm expectation that we would expedite our rollout process,” as Patrick puts it).
And so just as NHS organisations suspended elective care to deal with the coronavirus crisis, so too did Consultant Connect stop any activity deemed non-core to its fundamental central mission.
“What happens as you go along you develop a variety of things to improve your product. Some of those things are core and other things I think of as Christmas lights – attractive add ons. But already in February we realised that the only thing anybody is going to remember about us in this crisis was if we were able to connect clinicians.”
It meant all attention and resource was concentrated solely on that central aim. “We abandoned all projects that weren’t about that, so any tech development that wasn’t about facilitating that communication. Anything that was non-core we jettisoned, and all we focused on was modelling different loads, seeing how our system reacted, and then making changes to our system to make sure it could tolerate the loads.”
This all-hands-to-the-pump philosophy enabled the fastest ever rollout of a Consultant Connect service: it took just 72 hours between the instruction to proceed with implementation at Swansea Bay University Health Board and the setup going live.
It’s a record Patrick suspects won’t be broken again, but he also does not anticipate much of a slowing of progress on remote consultation in the NHS. The total rollout of Consultant Connect across Wales – which was commissioned by the devolved government there – is almost complete, and he also speaks of advanced conversations with a variety of other areas.
“The NHS has an opportunity to advance remote care like no other,” he suggests, “because the public don’t want to go back to how things were. So previous flashpoints about waiting times in A&E; now we’re in a position where actually the public doesn’t want to go to A&E in the first place. We don’t know how long this is going to last. My suspicion is it’ll last until a vaccine has been found to be reliable, but it’s certainly happening now.”
That’s why he believes improved communication between clinicians is one of the most important areas on which CIOs and CCIOs can valuably focus their attention in the coming months.
“Sorting something like communication between secondary and primary care is the easiest, highest impact thing they will do in the next five years if they want to impact their patient care, flow and manage the upcoming winter,” Patrick contends.
“There will be loads of amazing tech-led projects that they will do over the next five years – things like electronic patient records, patient wearables, self-monitoring – but if they’re thinking about having as big an impact as they can as quickly as they can for as little money as they can, sorting out communication between primary and secondary care is going to be the best thing they do.
“GPs working with secondary care clinicians and then using their prescribing rights to implement the advice of senior specialists is so much better for the patient, but it’s taken Covid to realise just how achievable it is,” he concludes.
To find out more about Consultant Connect, visit www.consultantconnect.org.uk.
Website: www.consultantconnect.org.uk
Twitter: @ConsultantConn
LinkedIn: Consultant Connect
Contact: 01865 261 467
E-Mail: hello@consultantconnect.org.uk