Developing the real business case for digital pathology
- 15 September 2020
Former Northern Cancer Alliance Pathology programme manager, and now cancer patient, David Bottoms, explains how the business case for digital pathology is starting to come together.
NHS England announced in 2019 that nine trusts had come together to sign a contract with Swedish imaging company Sectra to build one of the largest scale regional digital pathology networks ever created in the UK.
Reaching this stage is a tremendous accomplishment and opens new possibilities for pathology services and patients alike, especially around capacity and speed for important diagnoses – including for time critical conditions like cancers.
When I first started working as the programme manager for the initiative, I was already passionate about its potential for dramatically changing the way regional pathology services operate and collaborate.
Then, after working with regional influencers to create a model, I was suddenly struck with cancer myself. All the things I had put in the business case suddenly became very real to me – and I am confident that if the digital services now getting underway in the region had been available at the time, that my own complex diagnosis would have been made earlier.
Now retired from the programme, my personal medical history is just one example of why digital pathology really matters to people, and it’s one reason why I’m determined to share the lessons of how to make it happen.
So how did we in the North East of England and North Cumbria manage to produce a business case that would make this reality?
Proving the concept
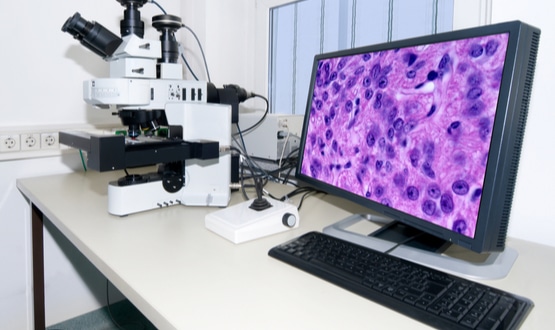
The project started when a group of influential histopathologists were interested in the new digital pathology scanners and wanted to try them out in their own laboratories, testing out the quality of the images and whether they could easily be viewed across the region.
Having been seconded at the time to what is now known as the Northern Cancer Alliance, I had been given a regional role to facilitate harmonisation of pathology services, and within this remit I took on the responsibility for managing the programme from its inception.
We began with a proof of concept in 2015, obtaining scanning equipment on-loan, free of charge from one of the major suppliers. Very quickly pathologists decided the images created by scanning slides were of a sufficiently high quality to make the vast majority of diagnoses. Pathologists agreed the proportion of cases that remained difficult to diagnose would have also proved difficult if they were looking at them through a microscope.
Finding the money
With pathologists satisfied digital would allow them to do their job and would improve case collaboration, services in the region concluded it was time to bid for funding. With capital funding scarce within individual trusts, we needed some form of prime funding.
The Northern Cancer Alliance was very supportive – and a bid for a pot of money around early diagnosis was successful, meaning we had approximately £2m to put in the initial tranche of funding to purchase equipment.
Making the business case
We then needed sign up to a business case from each of the then nine trusts that were on board at this stage in the project.
I created a regional template that set out the costs, anticipated start-up funding, and how much each individual trust needed to commit.
Importantly, we agreed at a very early stage how we would proportionate support and capital costs for each of the trusts. It wasn’t just a case of splitting it nine ways. We would look at their size, workload, and number of consultant pathologists, for example.
It was also vital to localise the business case. The pathology service in each trust took responsibility for tailoring the regional business case I had developed to their own needs. So, rather than me trying to convince everybody, we used the local pathology leaders to go to their IT managers, finance directors, chief executives, and chief clinical information officers, to make the case for change, why it would be so fantastic for the future, and why they needed to be part of it.
With that local groundswell and the fact that they knew they could come back to me with more detailed financial questions, we pushed this past the post before moving to a competitive tender.
But with so many people to convince, how did we persuade them?
Overcoming the IT hurdles
We came across IT directors that were very supportive, who could see this was the future. But many IT leaders also had their own busy agenda centred around core digital programmes like the electronic patient record. Pathology was an extra responsibility and claim on their resource, and so we needed to convince them it would work.
Though proven, digital pathology is still seen as a new technology. And unlike the digitisation of radiology, it is not backed by a national programme.
One specific hurdle we faced in the IT arena was around resilience. We originally envisioned a data storage efficiency on the basis that we didn’t believe a duplicate digital back up would be needed. Our back up would be in the original glass slide that could be rescanned in the event of an IT storage failure. Pathologists felt that was acceptable, but IT directors did not and insisted that a duplicate image is created at the same time as the original and stored separately.
Initially we feared this may double the storage cost and potentially derail the programme. But when we went to suppliers and asked what it would cost to duplicate the image on a million slides a year, it was approximately another 20-30% of the cost, owing to an economy of scale. Coupled with some additional funding made available by the Northern Cancer Alliance, we were able to make this affordable, and IT approval was gained.
Convincing finance directors
On the numbers, the ability to reduce costs of locum staff was key. Additionally, some trusts spend substantial amounts outsourcing pathology work to agencies, which in turn send at least some of that work back to NHS pathologists who receive payments from the private sector at a cost per case. However, the private agencies also add their own overhead charge.
Working digitally as a region would mean that any pathologists doing this work privately could instead do it directly for the NHS at the same rate, allowing us to cut out the agency overhead. So, this would mean a substantial saving for trusts on the principle that the extra work that couldn’t be done by ‘trust A’, can now be picked up by our own regional pathologists working for us privately as a network.
By investing in digital we believe we can also increase the overall number of pathologists we recruit reducing the need for paid overtime. A digitally connected region creates a far more attractive environment for new pathologists, who feel they are part of a more supportive network, rather than working potentially in a small trust, with no one to turn to help them in their field other than private companies.
Finance directors of course also considered other key factors – such as clinical benefits and risks mitigated against by investment.
Demonstrating the clinical benefits
There are too many clinical and quality benefits to describe in one article, but we believe that digital pathology will be a game changer for improving some aspects of the quality (ie simultaneously viewing different stains on the case tissue) and also the speed of diagnoses on the majority of cases. Running computerised algorithms to very quickly score slides for markers like HER2 (human epidermal growth factor receptor 2) will deliver a real time-saving too and could be triaged by non-clinical staff.
For complex cancers, a case will often get referred across two and sometimes three trusts. That involves packaging tissues and glass slides into a transfer box, moving it in hospital transport, unpacking the tissue by the receiving trust’s pathology department, and entering it into their workstream, where it then takes a little while before it gets looked at by the pathologist, who might then refer it again to a specialist in a further trust, for the loop to start over. Ultimately those tissues then need to be packaged up again and returned to the referring trust. All of this takes time and resource.
With digital imaging the pathologist in ‘trust A’ can see which other pathologists are currently online in region. If one of them is a thyroid specialist, for example, they can instantly be messaged – just like Facebook Messenger or WhatsApp, but also in a way that complies with NHS data security requirements.
The pathologist can ask their colleague to look at a specific area of an image, even a specific cell, and ask for their specialist opinion. If a further pathologist is required, they can put it into their in-tray and expedite it so it is at the top of the list. This can result in a clinical opinion in one or two days, instead of the one to two weeks that some cases can take.
Working digitally also means we can much more easily balance workloads, send the right cases to the right pathologist more easily, and ensure an urgent case isn’t sent to someone who is on holiday until next week.
We can audit cases far more effectively, help ensure pathologists haven’t missed something, and can start to use Artificial Intelligence (AI) to help us stage cancers and identify the hotspots for pathologists to look at.
It is much easier to do comparative analysis with historical images and different stains all on one screen – things that just can’t be done with a microscope.
And – we can make all information from one analysis immediately available to the next pathologist, as well as being available for the multi-disciplinary team meetings who no longer need to wait for slides to be loaded and navigated.
Scaling
The business case has been so compelling that other trusts have already joined the programme before go-live. Owing to a merger, we went from nine to eight trusts initially. But two trusts neighbouring the region in York and Hull have also joined the network.
Advice to others
To others looking to replicate our regional approach, I would conclude that our pathologists’ views were that digital imaging is proven to diagnose the majority of cases as well as a microscope and is the way forward.
Pathology departments are being expected to network, rationalise and standardise. Digital imaging can be a powerful tool to make that happen, to allow pathologists from different trusts to get together to share work, share standards, share teaching, and share audits and failsafe discussions.
Central to the success of any business case is to ensure all key stakeholders including finance and IT are engaged early. Digital pathology can bring together wide geographies, but the key is to make sure it is driven locally.





2 Comments
Our report Digital transformation: Shaping the future of European healthcare includes a case stud yon digital pathology in Italy – see Case study 4, page 27 http://www.deloitte.co.uk/europeandigitalhealth – if interested i could link you to them.
Hi Karen
This article does not refer to general digitization of pathology labs as in your report. It is about image digitization (WSI), digital pathology imaging.
Comments are closed.