The benefits of adopting a user centred design approach
- 8 October 2020

Matt Edgar, associate director of design and user research at NHS Digital, explores the benefits of adopting a user centred design approach, especially during a pandemic.
Responding to the coronavirus pandemic has been one of the biggest challenges the NHS has had to face since its inception in 1948.
NHS Digital has been at the forefront of the drive to improve services through data and technology and the pandemic has accelerated those changes faster than we ever expected.
However, despite the pace and pressure we are dealing with, we are still determined to put people at the heart of everything we do.
Everyone wants to enable better patient outcomes and make best use of scarce healthcare resources. This can only happen when services meet user needs, are inclusive, easy to adopt, and easy to use.
I’m sure you can point to cases where a lack of user research has resulted in the opposite: substandard services, wasting time that staff and patients don’t have, and money that taxpayers can’t afford.
Real life is complex, surprising, and more diverse than we can imagine. There is no substitute for hearing first-hand from people, especially those whose life experiences are very different from our own.
The pandemic has brought with it a whole host of challenges and we’ve been busier than ever. Nevertheless, we have been determined to double down on our principle of always putting the user at the heart of what we do.
Our teams at NHS Digital keep on discovering and applying the latest good practices and we think these user-centred design practices apply across the full range of services that we deliver nationally. They are also highly relevant to the many services that are commissioned and delivered locally in health and care systems up and down the country.
Good user experience starts by uncovering what people really need, in the context of their lives and working environments
Back in March, our team of user researchers suddenly had to switch from meeting users face to face to doing almost all their research remotely. I’m so proud of how they’ve done this – particularly of their efforts to reach seldom heard groups in society who are most at risk of being excluded from digital services, such as people of Black African, Black Caribbean and Asian communities who are disproportionately likely to be affected by coronavirus.
Researching remotely brings limitations. For some research we can’t wait to get safely back to physically meeting with users.
We have however also found there are some benefits in our altered ways of working. As a senior leader, it has never been easier to observe primary user research, just by tuning in on Zoom or Microsoft Teams. I’ve been privileged to see and hear people talking about their experiences of healthcare, and to watch them interacting with prototypes of new services, without having to leave my home.
Our products need to solve problems and reduce complexity – both individually and when we put them together into end-to-end services
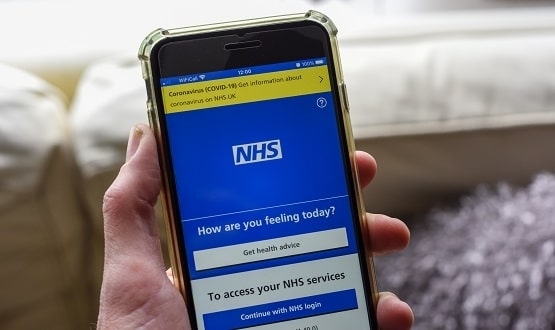
When the pandemic struck, our digital teams swung into action and created new services, often in a matter of days. Some of these were extensions to existing services, such as the NHS website and 111 Online. Others were brand new services, such as the Isolation Notes – announced in the Budget and live within a fortnight – enabling people to provide evidence to their employers that they needed to stay at home because they or their family had potential coronavirus symptoms.
Each new piece of work was done in a familiar user-centred way. Teams made sure they were solving the right problem, considered digital accessibility from the outset, and iterated – even faster than usual – to come up with usable solutions.
With all the new services linking to each other, there was a risk we were making things too complicated for people. When someone first had suspected Covid-19 symptoms, there was a lot for them to take in. Deciding what to do, in what order, could be especially overwhelming for someone who was feeling unwell, or fearful for their health, their loved ones, or their financial security.
Our community of designers, content designers, and user researchers collaborated on a new set of coronavirus pages for the NHS website. They tested different options with users to make this complex set of services, delivered by different teams, fit together more simply from a user’s point of view.
We must always have an eye on how our products and services deliver better outcomes
Behind every big launch and milestone, there will be multiple contributing factors, and hundreds of separate design decisions to make:
- Can people find the service?
- Do they trust what they find?
- How many start to use it?
- How many get to the end and achieve what they set out for?
- Who is in danger of being left behind?
By measuring the performance of our services in detail, teams can spot pain points for users, and identify opportunities for continuous improvement.
When our website stats suggest we might be losing users before they’ve finished a task, we can run usability tests and in-depth interviews to learn why that’s happening and how to fix it.
If we have a hypothesis that changing something would improve outcomes, a well-engineered digital platform makes it really easy to try out different designs and see what works best in real life.
For the sake of the patients, public, and staff we serve, we aim to work across organisational boundaries and continually learn how to do better together
If you’re a decision-maker in a health and care organisation, this is for you…
- in the future, when you deploy or integrate with an NHS Digital service, you can be confident that it has been designed and delivered in a user-centred way. If you find it has not, please let me know!
- when you’re buying a digital service or tool from a third party, you can point them to NHS Digital guidance and standards to show them what the NHS expects in the fields of accessibility and user-centred design
- if you already have user experience professionals in your organisation, we’d love to have them join our community
- if you’re just starting out and hiring your first in-house specialists, we’d be delighted to share what we’ve learned about how to recruit and on-board these essential new skills for your organisation
For those who want to get in touch to learn more, please email ucd@nhs.net or visit our NHS Digital Service Manual community page.




1 Comments
” . . . we are still determined to put people at the heart of everything we do.”
Excuse me, but this is a lie. You put IT at the centre of everything you do. You only consider people on the assumption that the solution they need is digital. Has it ever occurred to you to consider the possibility that what people need in healthcare is not digital?
I not very respectfully suggest that you are the problem, not the solution.
Comments are closed.