Measuring Digital Maturity– where is the value?
- 22 December 2020

Dr Jonathan Bloor, medical director at System C Healthcare, muses on the value of measuring digital maturity in healthcare.
Hard commercial imperatives and the need to stay ahead of the disrupters compel the banking, music and travel industries into a constant process of digitisation.
These commercial drivers just don’t exist for the NHS. Instead, measuring and benchmarking digital maturity has been devised as a tool to try and accelerate the process of digitisation in healthcare.
There is a significant difference in emphasis here compared with the commercial world. Although digital maturity measures have been developed in other industries, they tend to be linked to consultancy services which support businesses and their digital transformation. They have not been the major force behind digitisation.
The main model
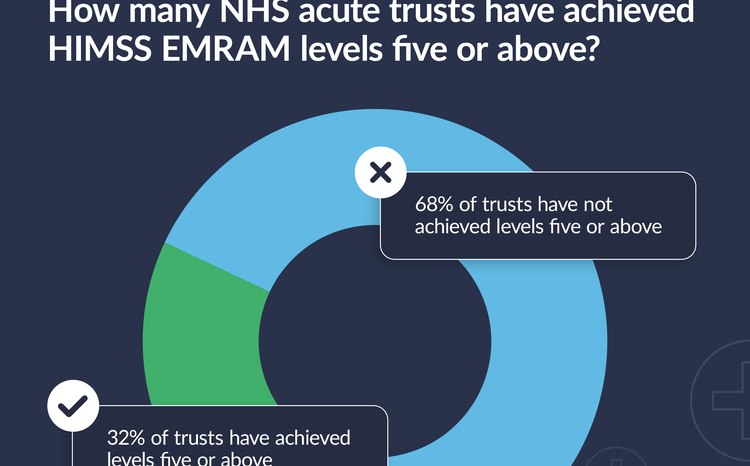
The predominant healthcare maturity model was developed in the US by HIMSS. It’s Electronic Medical Record Adoption Model (EMRAM) goes from stages 0-7 and describes the adoption and use of electronic health records by hospitals. The HIMSS model was originally developed for the US market, and there has been only a few announcements about NHS hospitals being accredited at HIMSS levels 6 and 7.
The NHS in England devised its own model thought to be more applicable to our public service. The Digital Maturity Assessment was used as part of the assessment process for the Safer Hospitals, Safer Wards: Technology Fund and the Global Digital Exemplar (GDE) Programme, but it now appears to have fallen out of favour.
Back in the forefront
Measuring digital maturity has its advocates and detractors and interest in measuring digital maturity inevitably waxes and wanes, but it does seem to be at the forefront of people’s minds once again in the NHS as we look at where next on how to target limited investment priorities.
We are also seeing renewed academic interest in the subject. Recent papers in Lancet Digital Health and the Journal of Medical Internet Research have questioned current approaches and have started to try and re-define digital maturity measures beyond individual hospitals and institutions, so the focus is broadened to system-wide transformation capabilities.
As the NHS starts to think again about measuring digital maturity there are some important things we need to consider.
What should be measured
Demonstrating improvement is important for staff, organisations, the system and the public, and this can’t be done without measuring. There is no question that when benchmarking is used effectively in healthcare it automatically drives improvement and tackles unwarranted variation.
However, there has to first be agreement about what should be measured, and the data has to be trusted and transparent. We have not reached this point of agreement yet and it is likely to be difficult to reach. If or when we do get there, it is important that the benchmarking of digital maturity is owned by Trust and Integrated Care System Boards, and not left to IT departments alone.
We should also recognise that current measures are focussed on organisations and not systems. In the UK we should instead now be focussing our digital transformation efforts on integrated care models and not the old hospital-centric model. The recent NHS England/NHS Improvement publication ‘Integrating care- Next steps to building strong and effective integrated care systems across England’ makes this very clear.
Addressing the problem
And we also need to address the problem that current maturity models mainly address functionality deployed and adopted, not value or benefits achieved. It is self-evident that we should focus on the outcomes that actually matter for the amount of money spent.
Only then will we understand if variation in spending on EPRs by NHS trusts is warranted. This is easier said than done, and the complexity perhaps highlights that digital transformation can no longer be seen as separate to healthcare transformation in general.
Creating the right market
There are other problems associated with the disproportionate attention given to functionality. First, a focus on specific functionality can stifle innovation. We need to ensure that we create a market with more choice, and not less.
Second, digital maturity scores can and have been used by organisations to ‘game the system’ by overstating or understating maturity to access funding. We need to make sure this doesn’t happen.
Third, current measures do not really focus on usability and workflows. An organisation might have ticked all the functionality boxes but not fundamentally transformed the way they work. The on-the-ground experience of clinicians will remain poor and benefits will not be delivered.
Finally, we need to make sure the measurement process itself isn’t onerous and a distraction from just getting on with the job.
Change is on the horizon
Ironically, over the last six months we have seen a sudden and rapid acceleration in digital maturity in the NHS as we respond to the new risks facing us. The intensity of this change suggests that failure to digitise the NHS is not really a technology problem or a capability problem after all, but is instead a matter of organisational and political will, together with operational imperative.
With attention turning now to a third wave, everyone remains focused on getting on with the job. There is a strong feeling that significant progress has been made in terms of digital support to the NHS and patients. When we have time to measure the improvement in digital maturity, it will be interesting to see how far we have come.




2 Comments
Some key points, absolutely spot on, in the latter part of the article. Planning and process change need to precede product selection and deployment, otherwise products just sit on the shelf. The next challenge is to then transform mainstream users, rather than focus on pathfinder success, in order to achieve true maturity
Brilliant article , right on the money. We need some kind of genuinely independent assessment. I tried to do something in this space 10 years ago during NPfIT but didn’t really have the bandwidth or money to make http://www.comparethesoftware.co.uk anything more than an idea. It really needs regular surveys backed by government strategy over many years to drive improvement. How much does EPIC/Cerner/Meditech RiO cost per user per month? And how do they compare on usability? Currently unknown. Can we really carry on like this?
Comments are closed.