Joe’s view: of Patient Online
- 20 May 2016
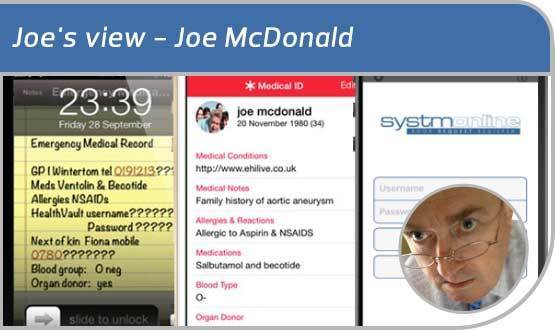
Back in October 2012, older readers may recall that I described creating my own emergency care record on my iPhone.
I did this by writing my basic medical history into the notes app, screenshotting the result, and using the picture as wallpaper on my lockscreen. I used this to record the fact that I have a potentially fatal allergy to aspirin.
The idea was inspired by Bob Brochtie’s ICE campaign, which encouraged people to store a next of kin phone number in their mobile phone contacts under the name ‘ICE’ – short for In Case of Emergency.
A publicity campaign encouraged paramedics to look for the ICE entry, and use it to contact people who might be able to share important medical information about an incapacitated patient.
Later Brochtie published an iPhone app which allowed people to display their key information on their lock screen. Remember the days when your mobile didn’t lock?
The latest thing: detailed care record access
In February 2015, Apple’s operating system iOS8 brought us the HealthKit app, which included a functionality called ‘Medical ID’.
This allowed people to surface their information on their iPhone lockscreen; but I was disappointed that it didn’t offer the opportunity to include a functioning hyperlink to the patient’s Summary Care Record or HealthVault account (well they wouldn’t, would they?)
Since then, the NHS Patient Online programme has encouraged GPs to allow patients to access their detailed care records. All practices were required to provide access to the detailed, coded record by 31 March 2016 – the coded data only, not text and documents.
I finally got around to going in to my GP practice last week to request access. I was given a form to fill in and told to come back with my passport and a utility bill; even though I have known Tanya, the receptionist, for 20 years, and our children were in the same class at school.
I was told it would take up to three weeks to complete the process. I asked Tanya if many people had asked for access and she told me I was the third. So not exactly killed in the rush, then?
The form included information about the risk of being coerced into sharing my record by, say, an abusive spouse and the importance of keeping my username and password safe –not as easy as you might think.
I was not issued with a smartcard. My GP uses TPP SystmOne and that has an iPhone app, which I have downloaded to my phone.
A small diversion
Last month, Emis went a step further and announced its ‘Share Your Record’ functionality.’ Share Your Record is part of Emis’ Patient Access online service. It allows patients to share a view-only snapshot of their record from a desktop or handheld device, via a secure URL or QR code and a four digit access code.
This has been criticised by my friend Ade Byrne as a gimmick, because it would require the patient to know the email address of the clinician who needed to view the record and because permission to view the record expires after 24 hours. He feels it is not a solution that will work at scale in the NHS. He’s right.
Nevertheless, it offers a tantalising glimpse of a patient-controlled sharing model that could deliver detailed information to clinicians at the point of care. Or beyond. The Doctor Online Programme?
Add a few boxes and sort the consent issue
As I already have to fill in a form to request access to my detailed care record, I might as well be given boxes to tick about my views on information sharing. These could be recorded in the GP system and on the NHS data Spine.
Am I happy for my information to be shared for direct care purposes within the NHS? Tick. Am I happy for my information to be shared for research within the NHS? Tick. Am I happy for my information to be shared with Google DeepMind? Errr, I’m going to need more detailed information about that before I can give informed consent – call me.
My log-in details arrived today. I navigated to the GP practice and a couple of interesting things happened. Firstly, I accidentally logged into my wife’s record because her username and password had been remembered by the family computer in the kitchen. Worth warning the patient about on that form, maybe?
Secondly, when I viewed my record , was a little surprised to see there was no record of my aspirin allergy. To be fair, I haven’t seen my GP for 20 years and the practice has changed IT systems in that time; presumably my allergy got lost in the move from paper.
Come to think of it, I was at university when I had my anaphylactic reaction; and my GP in Newcastle probably never knew about it.
In the Patient Online Programme of the future, maybe, at this point, I could enter the details of my allergy into my record and save the NHS a job? Apparently, the GPs are a bit busy at the moment.
As it stands, I will have to ring the practice and ask them to enter that information; even though I am logged in and looking at the empty allergy field.
One third of a lifesaving revolution
There may be only three of us looking at our detailed care records in Gosforth – and I now know my wife is 50% of the other two. But I’m sure those numbers will grow.
Three people hardly constitutes a scientific study, but as it stands 33% of them may have saved their own life by signing up and realising that they have a serious allergy undocumented anywhere in the system. Just me?
In only four years, we have gone from “ICE” to the patient having the ability to view and share their detailed care record on their smartphone. It has been achieved by putting the patient in charge of the consent issue for the sharing of their detailed care record; a principle which should be more widely applied.
|
Joe McDonald
|