Advisory Series: Interoperability
- 23 January 2019


Interoperability – Advisory Series, January 2019

By Maja Dragovic – Digital Health
Data sharing between primary and secondary care has long been a digital challenge for the NHS. But with Matt Hancock focusing his attention on resolving the problem and a new national programme underway, is a corner about to be turned? Maja Dragovic finds out.
Ask Phil Koczan to sum up where things stand on interoperability between primary and secondary care, and he speaks of a “transition phase”.
A practising GP for more than 20 years – and now also clinical director for health and care at the Professional Record Standards Body (PRSB) – Koczan has been around for various national pushes on data sharing between the two sectors.
Jeremy Hunt went as far as to visit specific GP suppliers to urge them to improve the data sharing of their systems. His successor as secretary of state for health and social care, Matt Hancock, has also singled out interoperability between primary and secondary care as a real problem.
But speak to Koczan and he explains that, in his area at least, the technology is now there to share information. “We’ve now got the technical capability to share the data records. As a GP [in Chingford, north east London], I can access the hospital records and the hospital can access some of the GP data. So, technically it’s possible.”
Good examples
Indeed, he says local data sharing programmes in his area are working well. “All documents are shared, all referrals are done electronically, information that comes back to practices is increasingly sent electronically, and we’ve got that wider record sharing up and running.”
Technology has also enabled GPs to see all the tests organised by hospitals and the results of those tests.
“We open our patient record and press a button that will show us what information is held by the hospital on that patient”, Koczan explains. “It could give us recent admission, any attendances, investigation results, and hospital appointments.”
Working both ways
Which is clearly all good progress. But is the data flowing in both directions – from GP to hospital as well as from hospital to GP? Not always, it seems.
“We have a relatively superficial view of the GP record,” reports Geoff Hall, medical oncologist and chief clinical information officer at Leeds Teaching Hospitals.
One of the reasons behind this could be that some GPs are reluctant to share their data because of uncertainties surrounding information governance.
“Doctors have been told all their practising lives that all the information should expressly have permission in writing to share it but that is no longer the case,” Koczan points out.
This leaves many GPs uncertain on what they can share, how they can share it, what consent is needed, or how the general data protection regulation (GDPR) applies.
“Everyone has a slightly different understanding of what’s needed,” says Koczan. “There are national guidelines, but it is often the local implementation that causes problems. They may be interpreted locally, or it may be that different systems haven’t got the ability to enforce the rules.”
And there can be challenges too with that old NHS chestnut – budgets and who should pay for what. Who should cover the cost of installing data sharing setups between primary and secondary care? Is it the CCG, the hospital, the local health economy more broadly? And where will the finance come from?
Koczan argues that hospitals shouldn’t pay for a system which everybody else can get benefit from and that this should be a shared responsibility. He hopes the new Local Health and Care Record Exemplars (LHCREs) may help here.
GP Connect
And there is hope, too, that another nationally-led initiative may help make a difference with primary/secondary care interoperability. Last summer, Leeds became the first city to go live with GP Connect, an NHS Digital-led programme designed to make it easier for clinicians across care settings to view a patient’s GP record, manage GP appointments, and access data on a patient’s medicines and allergies.
“The main benefits for this are for secondary care users, where it is offering an enhanced and much richer view of GP records,” says Alistair Walling, chief clinical information officer for Leeds City Council and Leeds CCG. “These users in particular have reported some individual cases of really positive benefits.”
One such case is when a patient was admitted to hospital with pancreatic cancer diagnosis established by the GP but “the hospital notes were literally empty on this patient apart from the investigation results”, explains Hall.
With GP Connect, however, he was able to read the notes made by the GP – and so know exactly what had already been explained to and discussed with the patient.
“Having access to that information, I was able to walk into the room and say: ‘I know all about the conversation you’ve had with your GP yesterday, is that still how you feel?’
“When the patient said yes, we were able to start managing him in the way that he wanted. We would have got there eventually, but we would have put the patient through a repeat of a clearly painful conversations for the patient and his wife, when we demonstrated that there’s absolutely no need to do that just by effective sharing of information.”
For Hall, the crucial addition to the new system is that it contains the plain text of the GP consultation – so increasing the ways in which the information can be manipulated, viewed and used.
One source for all
Though the initial functionality is clearly a step in the right direction, Hall is already contemplating the next stage. The plan, he says, is to integrate that GP data directly into the hospital record to merge information from two sources into one simultaneous display.
“At the moment we look at the data in the GP system and then look at the data in the hospital system. What I’d like to do is look at the information, see a list of medication and have some references to whether the medication is known about in both the hospital and GP system, not to have to look at the medication list twice and try and work out if there are differences between them.”
Hall also believes that there should be a single integrated community health record where all clinicians involved in a patient’s care would be able to enter data into one single system.
“At the moment there is this fear that a GP couldn’t possibly enter data into a hospital system and a hospital consultant couldn’t enter data into a GP system. My aspiration is that we break those barriers down.”
NHS diagnostics must embrace unprecedented openness if AI is to work

By Jane Rendall – MD, Sectra UK and Ireland
NHS IT vendors can no longer ignore technology they didn’t invent, and trusts need to integrate imaging far beyond the radiology department, if AI is to play its big role in diagnosing illnesses, writes Jane Rendall, MD, Sectra UK and Ireland.
There is no way Sectra could ever hope to develop even a fraction of the potential of artificial intelligence in diagnosing illnesses. It might sound strange for an NHS diagnostic technology provider to start a comment piece by saying what it can’t do. But this is a reality that all technology vendors face and must act on if the NHS is to realise the new ‘tech vision’ launched by the health secretary in October 2018.
The Department of Health and Social Care’s vision argues that artificial intelligence has “huge potential to improve diagnosis”. This is absolutely the case. But that potential will only be realised if another key facet of the same tech vision – interoperability – extends to the ‘ologies’, and to the imaging technology on which they rely.
Suppliers need to be open to AI algorithms from anywhere
A momentum for the NHS to move beyond outdated technology is building, and if vendors of traditional IT are to survive they must support the integration of all sorts of innovations into their offering. If they don’t do this, they will go the same way as the fax machine, and sooner than they might think.
Remarkably, whilst many companies are thinking collaboratively, we still live in an age where some diagnostic med-tech hardware suppliers force hospitals to purchase their own software to use on their modalities.
Now is the time for suppliers to be open, not archaic. Vendors can’t block the NHS from accessing innovations just because they didn’t invent it. And the same applies to innovations in the AI space.
Right now, within the NHS, and in companies across the globe, people are developing applications and algorithms to tackle real world problems – ranging from detecting deadly diseases sooner, to avoiding unnecessary appointments and encounters.
No single technology vendor could dream up even the smallest percentage of the ideas that innovators are coming up with worldwide. Yet, if you were to look across the competitive landscape in NHS diagnostic IT, you might often hear the same mantra from companies obsessed with their own algorithm developments, rather than the wealth of ingenuity they could embrace for their NHS customers.
This isn’t about what any one vendor is developing – and it is not about what Sectra is developing. The key is for suppliers of traditional technologies, like the electronic patient record (EPR) or the picture archiving and communication system (PACS), to ensure they are open and interoperable, and that AI applications demanded by their customers can plug in to the core technologies relied on in the NHS.
An open platform for AI diagnostics
Hospitals need their core systems to be open platforms for AI. Sectra is already working with hospitals to achieve this. We have a fundamental belief this is how we will be successful as a supplier.
If a hospital wishes to implement their homegrown application into their PACS to identify patients across their region at risk of cancer, they can do this.
Or if they want to implement an algorithm developed by another vendor or innovator to diagnose diabetes sooner, following necessary due diligence to ensure that application is safe, we will plug this in to the PACS.
This is our ethos – to enhance our core role around the flow of imaging and diagnoses in a way that is helpful to radiologists, pathologists or any healthcare professional – by building on this as an open platform that allows AI to securely flourish for the benefit of professionals and patients. And we will continuously work harder at this, so we can make sure we can give our NHS customers the opportunity to take advantage of the newest technologies that can make a difference.
Leaving silos behind
Really making this work however means applying AI to the richest dataset as possible. That doesn’t necessarily have to mean sharing data externally, but it certainly necessitates joining together data and imaging across the trust, and thinking at the population level.
Simply put, the NHS can’t afford to keep investing in departmental radiology PACS for hospitals if it is to expose its new AI applications to the data they need to support effective diagnoses.
Enterprise wide image management is the only way forward, where the barriers across the ologies are broken down, so that images from a whole host of diagnostic specialities can support diagnoses and become integrated with information from the EPR.
Standards such as HL7 FHIR, or Fast Health Interoperability Resources, can be key in enabling this, but again, this does require willingness from vendors to collaborate, and for the NHS to think differently about a strategy for digitising images and information.
Only then can AI be used to look for patterns in data, to identify incidental findings that might show the early onset of a disease not originally being searched for, or that can help to determine how a catastrophic event in A&E might be avoided.
These are real world problems, but only through a genuine interoperable and open approach from the NHS and its suppliers will they be solved.
|
|
| Contact number: 012 7921 3653 Email: caroline.marjason@sectra.com Our website: www.sectra.com/nhs_integrated_diagnostics Twitter: @SectraNews LinkedIn: www.linkedin.com/company/sectra Further reading: A call for connected diagnostics Breaking down silos: Delivering true clinical value from a VNA [ssba]
|
|
The reality of NHS interoperability
By InterSystems
If we are to effectively tackle the unprecedented financial, clinical and social problems in health and care most people accept that we have to integrate our local health economies.
Renewed energy, ambition and opportunity
Health and social care secretary Matt Hancock has undoubtedly injected new energy into the integration agenda – not just with the promise of money for technology, but with a documented vision for national approaches.
Hancock is a believer in technology and is prepared to stake his faith in it to solve many problems. He expects the NHS to do the same and wants to see next generation technology available to staff that integrates information across care boundaries. These technologies will be underpinned by “strict, mandated, open standards for interoperability of systems”, and all suppliers must support the required change.
Hancock is not the only key figure supporting technology investment for integration, Lord David Prior, chair of NHS England and of University College London Hospitals NHS Foundation Trust, admitted that integration was absolutely needed and that providers needed to stop acting as “islands in the sea”, instead working together to help their populations, neighbours, and wider patches.
It is encouraging to see such clear indications of intent, particularly when you consider that nearly 10 years ago the straight talking IT analyst Boris Evelson wrote a blog after visiting HIMSS 2009 called “Healthcare Industry BI Groundhog Day”. And here we are nearly 10 years later asking the same questions:
- Where are the open technology standards?
- Where is the transparency?
- Where is the common sense that business requirements, not vendors, dictate the rules?
Even though we haven’t made as much progress as we should, we can be more optimistic that there is an alignment happening between the centre (NHS England, NHS Digital), the health and social care service and suppliers. We are on the cusp of doing something great, even if that means we are talking years, because increasing interoperability maturity and capability is a continual process – a journey, not a destination.
Long term investment
To aid that journey the NHS was promised an additional £20 billion a year in the Budget – but we all know the money will not go far. NHS Improvement has disclosed that the underlying provider deficit is now £4.3 billion, and there will be tension between getting hospitals back on track and delivering on the promises in the long-term plan.
Transforming services, implementing new models of care, is the only way to eliminate the deficit and make organisations sustainable in the long-run. We are seeing the development of payment models that put more emphasis on prevention, now we need the interoperable systems that will enable information to flow across the system, so patients can be treated in the right place and treated right first time.
When it comes down to it, the service can’t afford not to do this. And it has a mandate. Matt Hancock told the Health and Care Innovation Expo: “I am not looking for people to blame. I am looking for people to lead.”
Seizing the opportunity
Interoperability provides an unprecedented opportunity to standardise, re-engineer and improve clinical workflow. We have a responsibility to take advantage of this opportunity, and not to, would render the investment in interoperability useless. We must use new technology and models of care to change the way care is delivered – “old process plus new technology = extremely expensive old process”.
But how do we do it? Integrated Care Organisations (ICOs), Local Health and Care Record Exemplars (LHCREs) and forward-thinking health economies, now driving the interoperability agenda, realise they have to move away from the “break-fix” model of healthcare to one of prevention and continuous care.
Technical challenge or something else?
With this renewed momentum and a genuine opportunity to act on well-rehearsed arguments that favour integration and interoperability we should not pretend the interoperability needed will be easy.
Dr Graham Evans, the chief information and technology officer at North Tees and Hartlepool Hospitals NHS Foundation Trust, told the Joined-Up Health and Care conference this summer that the challenge to achieving real integration and interoperability is 10% technical and 90% everything else – people, process, culture and organisation. This applies just as much to achieving interoperability across a region as it does across an acute trust.
Make no mistake, there are huge challenges in “the 10%” technical work that must now be overcome quickly, but our eye must be on “the 90%”. This is integration of the next generation.
 |
|
| Contact number: 017 5382 9647 Email: Erica.Bennett@InterSystems.com Our website: www.intersystems.com/uk/industries/health-and-care/nhs/ Twitter: @InterSystemsUK LinkedIn: www.linkedin.com/company/intersystems-uk/ Facebook: www.facebook.com/InterSystems/ Further reading: HL7 FHIR and the Future of Interoperability (The other) Hancock’s Interoperability Insights: Vision without execution is just hallucination [ssba]
|
|
Application-centric and data-centric interoperability
By Marand
Healthcare is undergoing a transformation to an integrated, multi-provider model where the patient or more appropriately the citizen sits firmly at the centre. The focus has clearly shifted from individual care episodes to continuity of care and finally to holistic, population health management. It is not individual providers but governments at municipal, regional or national level that are starting to coordinate health and social care to help manage a citizen’s wellbeing.
This change in focus has many implications for IT systems, an area where healthcare providers already struggle. Clearly, the systems of today need to change since IT is a key enabler of this shift and interoperability is at the core of this challenge.
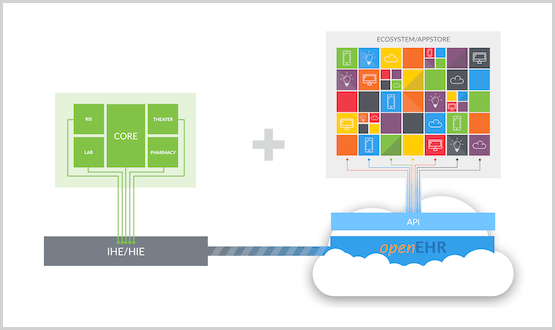
When it comes to health data interoperability, there are two schools of thought: application-centric and data-centric. The first believes that since there are so many systems already in place, we should agree on the exchange format (and recently the APIs) and convert the proprietary data into that format as needed. This is the preferred approach today when faced with a large installed base of legacy solutions. The focus here is on the applications.
The second approach is normalising the health data first, building new systems on top and avoiding the interoperability issues altogether. This entails defining a data layer, which is the most important aspect of an open architecture. Why is this the most important layer? Most healthcare organisations are beginning to realise that their data is more valuable than their applications. Data has become a valuable asset, since good data is key to improving outcomes, managing chronic disease and enabling population health management. The focus shifts from applications to data, i.e. the data-centric approach.
To do this, storing the data in a vendor-neutral format is crucial. Almost all applications store data in proprietary formats and healthcare is no exception. What is different in healthcare is that we need to keep data for the lifetime of the patient. It is clear that no application will last this long so we will be migrating data from one proprietary format to another every 10 to 15 years when replacing applications. PACS is a good example. The DICOM format was chosen 30 years ago and today, no vendor stores images in other formats. But unlike images, structured clinical data is still being kept in the silos of the applications that produced it making data unavailable to others.
While this problem has been well known for decades, it is now centre stage driven by the transformation of healthcare. A year ago, Gartner Group published a research paper named “A Roadmap for a Citizen-Centric Integrated Model of Care” where they clearly state: “Gartner believes that truly effective and sustainable open architectures will need a capability for vendor-neutral data persistence, such as utilizing a common schema or set of archetypes and rules for managing structured and unstructured data (for example, a VNA, openEHR or IHE XDS repository in combination with services for trust/consent, ecosystem governance and oversight, and reuse of data and processes for secondary purposes, such as research and population health). Providing open messaging standards (for example, FHIR, HL7) for data exchange in specific use cases will only go so far in meeting the architectural challenges of digital citizen-centric care delivery.”
So how do we get from an application-centric view to a data-centric one? Let’s take a look at the three steps:
1. Integrate
Most healthcare providers have many, many applications. When the GDPR directive came into force last year and providers had to catalogue their systems, larger trusts discovered they had hundreds of applications. All of them have patient data. All in a vendor’s proprietary format.
In order to make the best use of it, data needs to be extracted to build a lifetime health record describing the health status of the patient as accurately as possible. Using integration engines, data dumps, messaging or APIs, data is collected from as many applications as possible. Of course, this is a process and will not happen overnight. The first step is to focus on one or two areas where you are looking to innovate by buying or building a new app or application.
2. Open
Once you have access to this data, normalise it to a vendor-neutral format and cross map different coding to standard terminologies. This means using standards like openEHR for structured data, IHE XDS for documents and DICOM for imaging as Gartner suggests.
Other sources, like the NHS Apperta “Defining an open platform” whitepaper state: “openEHR is the only currently available open standard for the representation of fine-grained structured clinical content that is sufficiently mature and proven at scale.” Also “IHE-XDS and openEHR work well together, and this combination has been used successfully at scale. XDS handles unstructured and semi-structured data while openEHR handles fine-grained structured data with links between the openEHR clinical data repository and the XDS VNA enabling the creation of a seamless record.”
3. Innovate
It’s now time to take advantage of this consistent, longitudinal record to enable innovation.
How do we do innovation today? – we build a feral system! On the positive side, because they are driven by end-users, feral systems fill many gaps, are developed quickly, solve real problems and can also be very innovative. They often become essential for users to carry out their daily work. But there is another side to feral systems. For one, lack of integration with core systems prevents the sharing of data, requiring users to enter the same data repeatedly. Think about GDPR compliance and lack of governance. While innovative, feral systems are often not built or managed properly and thus pose serious risks to organisations.
What if you could buy or build new, innovative apps and put them on top of consistent data? Think patient engagement, precision medicine, clinical decision support, pathways and guidelines and how much easier it would be to build these solutions on a common data layer using predictive analytics, algorithms, machine learning and AI! You could now build an ecosystem of apps and applications which share data without additional integration. As long as apps commit to accessing and storing all data in this patient record, you can grow the ecosystem, taking advantage of innovation from different vendors. This architecture is fuelling the next generation of solutions known as the Postmodern EHR.
Conclusion
As mentioned above, most healthcare IT today is application-centric. To unleash innovation, IT has to start moving from the current state to a data-centric world. This requires three fundamental steps: integrate, open, innovate: use interoperability standards to integrate existing systems and data. Storing data in an open, vendor-neutral format will then enable ecosystems of vendors to innovate.
To see evidence of success with this approach, we need to look at the early adopters: countries like Slovenia and Norway, cities like Moscow, trusts like Plymouth, Taunton, Salford Royal and South London and Maudsley.
Remember: Integrate. Open. Innovate!
 |
|
| Contact number: +386 1470 3100 Email: info@marand.si Our website: www.marand.com Twitter: @TEHRplatform LinkedIn: www.linkedin.com/company/marand [ssba]
|
|
Interoperability – the bedrock of our future NHS

By Dedalus UK
Matt Hancock on his appointment as secretary of state for health and social care put interoperability firmly at the heart of his vision for the NHS. Whilst the ‘Five Year Forward View’ has been driving towards integrated care across all care settings for some time, its transformation funding was largely sucked into the hospital sector because of pressures in secondary care.
With the announcement of the NHS Long Term Plan the real prevention work out into primary care and the community can now truly take shape, with technology as a crucial element in driving productivity improvements.
Interoperability is core if this technology is to ‘transform the way we engage with the NHS’ and ‘improve the way care is delivered’.
Standards
Whilst the NHS Long term Plan provides a real-term, potentially ring-fenced, funding boost for the community, mental health and social care settings, the reality of disparate silos of information is still a very real hurdle for integrated care.
Matt Hancock’s focus on open standards to ensure the full interoperability and accurate translation of data between disparate systems is fully supported by Dedalus. As an active member of INTEROPen and with an R&D programme committed to open data, Dedalus solutions encompass the latest global healthcare standards – such as SNOMED CT for clinical coding, NHS dm+d (dictionary of medicines and devices) and HIE, HL7, FHIR and CDA2 for full information sharing.
Vendor neutral platform
X4H is part of the 4Health Solutions portfolio from Dedalus UK and is a vendor neutral, interoperability platform that consolidates data from many disparate health and community information systems to give a single, actionable patient record available across all healthcare users. X4H can operate on many levels from a foundation-level integrated record viewer to a platform for full population health management.
With 1.4 million NHS staff, 1.5 million local government personnel and a huge raft of disparate systems and processes both within healthcare and out into the community – fully integrated care may seem a monumental task. But with over 40 full scale global interoperability installations and more than 120 interfaced solutions, at Dedalus we are adept at solving complex challenges across entire care communities.
Multi-directional workflows
Unlike most conventional interoperability platforms which offer only mono-directional data flows (i.e. simple data aggregation), X4H, even in its basic out-of-the-box configuration, enables multi-directional workflows to give true interoperability to clinicians, laboratories, pharmacies, mental health, GPs, community staff, etc. – all within strict security and privacy protocols. It also has the ability to empower patients to take part in their own care process via Patient Portal applications.
Core functionality
X4H is Dedalus’ foundational interoperability engine, the enabler that brings third party systems together through seamless data integration. Built around the latest global healthcare standards, including IHE, HL7, FHIR and CDA2, it allows healthcare organisations to share and exchange information and future-proof against emerging integration patterns.
The full interoperability platform comprises:
- Integration engine – that allows both micro (within a discipline) and macro (cross specialty) interoperability across all third party systems
- eMPI – a central master patient index that consolidates patient IDs and demographics data, from widely disparate systems, to ensure accurate patient matching and care record completeness – eliminating duplications and misidentifications
- Document & clinical data repository – that provides a single source for all documents, events, images, tests and historical records
- Terminology engine – which ensures that disparate coding methodologies can be accurately matched against each other – including dm+d, SNOMED CT – for precise patient care
- Policy and consent manager – that ensures patient consent and GDPR compliance, and gives legitimate users defined access to ensure full process governance across the care community
- Single sign-on authentication – gives streamlined access and reduces the need for multiple log-ins
Health Viewer – our entry-level, web-based solution is HTML5 compliant and gives clinicians access to this invaluable data repository from a variety of handheld and static devices.
A true digital partnership
‘Putting the patient at the centre of the digital health experience’ is vital, according to Juliet Bauer, former Chief Digital Officer for NHS England. At Dedalus our aim is not simply to provide technology solutions and walk away. We work in partnership with our clients and their clinicians to deliver true healthcare transformation that produces better outcomes for both patients and staff. We are:
A dedicated partner committed to clinical excellence
Dedalus is at the forefront of new solutions development and is #3 KLAS-rated for new clinical projects worldwide – with over 3,000 global customers on 4 continents, in 25 countries.
Integrated clinical pathways
With a wide range of expertise in multi-site ‘hub and spoke’ laboratory networks, complex electronic prescribing and pharmacy installations or cross-boundary health and social care implementations, Dedalus enterprise-wide care planning and new clinical pathway development can facilitate a smooth transition in virtually any clinical environment.
Our X4H Clinical Workflow Enhancement module enables well-recognised pathways to be pre-set into the system, allowing secure, event-driven alerts to be delivered to the next carer in the process.
Practical change management
The challenges of establishing effective care pathways with strict clinical and information governance across such disparate audiences cannot be underestimated. Human and organisational processes are often well embedded and need skilled, perceptive, proven management to make the transition to full interoperability. Taking into account all stakeholder needs, while harnessing the full potential of the workforce and any existing systems is what Dedalus does best.
Population Health Management
The demands nationally are now for record sharing across whole populations such as in the Local Health and Care Records Exemplars (LHCRE) and CCG/STP projects in order to drive real population health improvements.
Our Business Intelligence and Analytics module forms one of the core components of our Population Health offering. It allows for a real-time glimpse into any organisation’s performance – both clinical and financial. Users can identify and monitor critical subsets of their population to set clear care parameters and drive health initiatives.
Digital innovation
According to Theresa May the focus now is on digital innovation to ‘harness the power’ of the workforce and ‘expand the boundaries of what the NHS can do in the future in the fastest, safest and most ambitious way possible’. Current examples of this include the approved NHS Apps Library, the NHS Login for digital access to personal care records, digital appointment booking and consultations, and Open APIs for new solutions integration.
At Dedalus our stance is to ensure that any new developments can be quickly integrated into our fully functional interoperability solutions so that immediate value can be realised and we can begin to see the true potential of the empowered consumer in health. Innovation is moving fast – so must we!
 |
|
| Contact number: 012 1638 0860 Email: ann.braham@dedalus.eu Our website: www.dedalus-uk.com Twitter: @DedalusUK LinkedIn: www.linkedin.com/company/dedalus-healthcare-limited Further reading: Dedalus Interoperability Platform [ssba]
|
|
Interoperability – from design to go-live in just seven weeks
By Orion Health
The lack of interoperability of data and systems has been a significant blocker to the delivery of integrated care for years. It has caused the pursuit of a single view of patient information to be difficult and dependent on the willingness of vendors to work together. It has largely been the job of NHS organisations to put pressure on their suppliers to make data available, with no formal incentive coming from the centre. There has been an absence of widely accepted data standards, making interfaces costly to build and not repeatable.
The good news is, this is changing. Orion Health is a founder member of the INTEROPen movement, dedicated to the development of open standards for interoperability in the health and social care sector. This group has achieved a huge amount since its creation in 2016, including a library of HL7® FHIR® resource profiles and interaction patterns (APIs). These include Care Connect APIs developed with NHS Digital. This movement has been voluntary and driven by those passionate about making interoperability a reality. So, it’s encouraging to see in the recently published NHS Long Term Plan that commitment to interoperability will no longer be a choice for vendors, in that compliance with published open standards will become a formal requirement.
Reducing drug-related deaths in Bristol, South Gloucestershire and North Somerset
So, why is interoperability so important? Is there a real-life use case of it improving efficiency and care? Yes. The Connecting Care Programme based across Bristol, South Gloucestershire and North Somerset has provided an integrated digital care record since December 2013. Since the initial go-live, many new integrations and functionalities have been added over time. Last year, the team had an ambition to reduce drug-related deaths for the homeless and vulnerable by bringing information on prescriptions for Opioid Substitution Therapy (OST) drugs into the integrated digital care record.
To meet this ambition, Connecting Care worked with Orion Health’s pioneering integrated digital care record and the Cyber Media drug and alcohol system, Theseus, which is used by Bristol City Council. To our knowledge, the project marked the first implementation of a Care Connect API in England. The project was very rapid, going from design to go-live in just seven weeks. The new FHIR supported interface can be viewed by staff working in 27 organisations, including 85 GP practices, NHS hospitals, mental health and out of hours services, social services, paramedics, charities and hospices.
This project proves what can be achieved when we embrace open standards and work together for the benefit of the patient. FHIR® is by no means a magic bullet, but it is only by using these emerging standards that we can refine them and move forward. This is complex stuff, but we are so much further ahead than five years ago when we were still discussing who owned data, and what could be shared, and what standards should be used for any sharing that took place.
Are you looking at implementing an integrated digital care record?
If you are looking to implement an integrated digital care record and to ensure that your project is at the forefront of interoperability, get in touch with us for a demo.

|
|
| Contact number: 087 0486 8406 Email: emea-marketing@orionhealth.com Our website: www.orionhealth.com/uk Twitter: @OrionHealthEMEA LinkedIn: www.linkedin.com/company/orion-health Facebook: www.facebook.com/orionhealth Further reading: Connecting Care goes live with a Care Connect API for safer prescribing Setting care transfers on FHIR [ssba]
|
|






1 Comments
Between me and my husband we’ve owned more MP3 players over the years than I can count, including Sansas, iRivers, iPods (classic & touch), the Ibiza Rhapsody, etc. But, the last few years I’ve settled down to one line of players. Why? Because I was happy to discover how well-designed and fun to use the underappreciated (and widely mocked) Zunes are.
Comments are closed.