Salting the record
- 1 October 2014
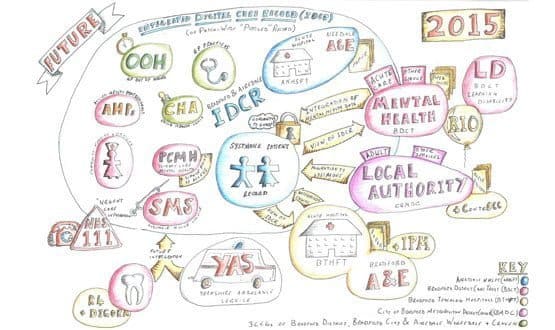
At Bradford District Care Trust’s offices, the Bradford and Airedale integrated digital care record programme board is busy working on a project to join up health and social care.
So busy, in fact, that its members barely seem to notice the sunshine reflected on canal outside its offices in the famous Saltaire Village; one of the homes of the industrial revolution, and a world heritage site.
That may be because the electronic, ‘path-wide’ record reaching across primary, secondary and social care is within reach.
“We have a track record of working together over a number of years,” says Dr Andy McElligott, medical director of Bradford District Care NHS Trust and chair of the IDCR programme board.
However, he says the time has come to do this electronically in a “more joined up fashion”. That was the reason why Bradford put in a £1m bid for NHS England’s ‘Safer Hospitals, Safer Wards: Technology Fund’.
The bid was successful and the project was picked by NHS England as one of three integrated digital care record exemplars. “This project is simply a tool to expedite the process,” says Dr George Eskander, a local GP and LMC representative.
Social care in at the outset
A number of organisations are involved in the project. As well as Bradford District Care Trust, Airedale Hospitals NHS Foundation Trust is on board, and so are the three local clinical commissioning groups: Bradford City, Airedale, Wharfedale and Craven, and Bradford Districts.
Bradford Council is one of the drivers of the vision and a major player in the project. Bradford Teaching Hospitals NHS Foundation Trust is involved, even though it was a silent partner in the bid.
Yorkshire Ambulance Service NHS Trust, the local out-of-hours providers, specialist services and the third sector will also take part in due course.
“How we’ve traditionally shared information has been on chunks of paper, but a lot of patients require care from more than one organisation at the same time,” says David Worth, programme director for digital care in Airedale. “All these different providers need to understand what’s going on with those individuals.”
Kathryn Lamb, project manager at the council says that information is not always passed effectively between health and social care providers and it makes it difficult to find out which care interventions are already in place.
“So much time is spent by social workers chasing information from health, and a large number of calls we get, are from health professionals wanting information about their patients,” she says.
Working with SystmOne
Most of the local health economy already uses TPP’s SystmOne as its clinical system, so it has been a natural step to use that as the basis for the shared record.
However, Dr McElligott points out that that the project is not about a single system or a single record. The programme board calls it a ‘pooled record’; through which the right information about the patient will be available at the right time to the right people.
“What’s true is that SystmOne has a major market penetration in the local area. It’s used by most GPs, and used by Bradford District Care Trust for the community,” Dr McElligott says.
It is so well used in fact, that the council has recently procured SystmOne as its new clinical system for adult social services.
“We undertook an options appraisal that considered linking our existing systems or moving to share a single system. We decided that our strategic and operational requirements were better met by a full migration to SystmOne,” says Lamb.
“In a shared system, different care professionals can more effectively collaborate when assessing an individual’s needs and we can then better co-ordinate our response to those needs.
“From the local authority’s perspective we’re currently in our implementation phase and plan for the system to go live on 1 April next year. TPP is in our organisation at the moment shadowing our service so they can undertake our development to ensure the system meets all our requirements.”
Bringing in RiO
As a mental health trust, Bradford District Care Trust itself uses the RiO EPR, and part of the programme is to upgrade that system so it integrates “in a meaningful way” with SystmOne.
Ian Lockwood, the trust’s IM&T project director says it is important to make sure that SystmOne users can see useful information in RiO and vice versa.
“It’s got to be real time. That’s the ambition. What makes it more complicated is the reality is that there are systems out there that are quite different – and there isn’t one system that does everything,” he says.
“SystmOne doesn’t currently have what’s required to deliver mental health service and they don’t do anything in support of dental services. Dental is another specialist system that needs to be bought in.”
The trust has been working with ReStart Consulting to use the InterSystems Ensemble integration engine to address some of these issues (the former Yorkshire and the Humber strategic health authority bought both Ensemble and consulting services for this kind of work).
The result is a first of type “integration communication solution” to share information between SystmOne and RiO.
Lockwood said the trust is also procuring mobile devices, most likely laptops, so staff can get access to clinical information in the patient’s home. However, these require a mobile signal, which in some areas is non-existent.
“There are areas in Bradford and Airedale where we don’t have mobile signal. But we can still enter data into the system and when we got access to the internet it updates it,” says Lockwood.
Practical results in place
Exactly how the full integrated shared record will look is something yet to be established, but each organisation is working on individual projects that will make this all add up to one big, shared project.
“We got to remove the disconnect between the different services, but we won’t have a glorious big bang. It will happen with different functionalities at different times,” says Worth.
By way of an example, he says that Airedale Hospital has recently gone live with e-discharge summaries to GPs. This includes getting notes from primary care and clinicians can actively “re-prescribe” medication noted in the record.
“If a specific brand is used in primary care, the decision support helps with the translation. Primary care can see what secondary care has done in their record,” says Worth.
Airedale also uses SystmOne and is now looking to roll-out electronic prescription and medicines management across the hospital, using the system.
“We are also negotiating with TPP on service requesting, which is for staff to request interventions, but that’s early days and we need to build a little more momentum,” Worth adds.
From a primary care point of view, Dr Eskander says any step towards joining up the care pathways is a welcome one.
“We have 100 GP practices; you can imagine how there is potential for communication between different agencies to be quite fragmented,” he says. “This is an attempt to implement care across the whole area in a way that helps the patient.”
Working for patients
When asked why the team has decided to put so much energy into the project, its members answer in unison: “Because of the people of Bradford and Airedale.”
They expect that there will be an op-out for patients, but the mechanism of that is something that is still being looked into.
“That’s the next bit of work and we hope that will clearly describe the information governance arrangement so that all of our people understand what’s being shared about them and with whom,” says Dr McElligott.
Behind the scenes, there is also further infrastructure work going on, such as improving standards and clinical coding so information won’t end up getting lost in translation. All of these pieces of work can seem fragmented, but they are all part of the joint strategy.
“We are equal partners in this. Each organisation has agreed the drivers for what it has got to do, but it is all underpinned by integrating care,” says Dr McElligott. “We all understand that there’s a big prize at the end of the day: the integrated digital care record.”




